Contents
“85 percent of companies report that their customers are significantly more digitally focused than they expected”, according to research conducted by Microsoft and The Futurum Group, global technology research firm[1].
With today’s multitude of data touch points ranging from email, text, chat, social media, apps, websites and more, connecting with customers can be overwhelming. To track this data and use it skilfully, you need a client engagement platform.
Client engagement systems are like your control board or dashboard that brings all that data together in one place. Essentially, it’s your marketing command center with all the data that relates to your customers including buying behaviors, demographics and more.
The client engagement tool solution then allows you to analyze and manage all that data to provide the optimal customer journey. For therapists and coaches, that also includes seamless invoicing, follow-ups and feedback check-ins.
Quenza is one such platform that allows you to easily send various forms, exercises, worksheets and reminders to your coaching or therapy clients. They also each get their very own engaging platform where they can access their messages, track their goals and complete their exercises.
As a client engagement tool software, Quenza is an all-in-one platform that covers your back office admin processes as well as your clients’ data. You can also set up groups of clients and store everything securely.
Why not see for yourself just how powerful and engaging Quenza is? You can get the full access for a whole month for free by signing up for the trial. There’s nothing to lose and everything to gain.
Chapter 1
The Rise of Client Engagement Solutions
Customers and clients are savvier than ever thanks to all the information they have access to online including chat groups and forums. Global word of mouth has increased their buying power in ways companies are still struggling to fully understand.
Traditionally, companies used third-party data to connect and engage with their customers. With today’s focus on data privacy, it’s increasingly difficult to access third-party information.
Moreover, more than 70% of consumers want to buy from companies that make the world a better place[2]. The impact of this social responsibility is that businesses can’t just rely on a great website or advert.
Instead, businesses need to leverage data-driven engagement. By working with client engagement tool systems, businesses can better understand their clients’ behaviors, preferences and interactions. In other words, what are their habits and what social issues do they care about?
If you’re a therapist or coach, your very essence is to make this world a better place by helping people. The art of using a client engagement platform is to leverage the data to connect with those people you know you can help and together, make this world a better place.
At its core, the role of a client engagement platform is to enhance your client relationships, as shown in the table below.
| Overview | |
|---|---|
| Accessibility and reach | You can reach anyone anywhere, whether they’re in a cabin on a mountaintop or on a deckchair at the beach. Those sceneries can create those moments of clarity when people realize how much they need a coach or therapist. |
| Personalization at scale | With AI, every email, recommendation or tip for the day can be tailored to each individual according to their profile and preferences. |
| Real-time interaction | Chatbots are there to keep people on your site or platform and can answer issues straight away before potential clients give up and go somewhere else. |
| Feedback loop & continuous improvement | A good client engagement solution needs an effective way to gather client feedback so that you can keep improving and adjusting accordingly. |
| Empowered clients | With a client engagement platform, you’ll understand just how sophisticated your clients are and what they expect from technology. You’ll then be able to give them what they want. |
| Community building | Engagement platforms also give you the opportunity to build communities. If you do group therapy or group coaching, this might be a particularly interesting feature for you. |
Chapter 2
Features and Benefits
A useful way to think of a client engagement platform is as a collaboration tool for your clients. In the same way that businesses share their vision, objectives and overall strategy with their employees, businesses now integrate clients into the family.
The more you understand your clients, the more they will resonate with what you offer. As a result, what you offer meets their needs and in return, you get increased loyalty.
As you can imagine, communication is top of the list when it comes to what makes a client engagement platform stand out. This needs to be through multiple channels such as email, chat, social media, calls or SMS at the very least.
With Quenza as your all-in-one client engagement software, you can access all those channels through your clients’ individualized portals. For example, the chat feature shown below is easily accessible at any time and place.

Feedback management is another critical component when it comes to finding the right client engagement platform. Again, with Quenza, you can easily send your customized feedback form through whichever channel you want.
Analytics and reporting are also key tools so that you can stay on top of your data and generate useful insights. For therapists and coaches, Quenza has goal tracking and invoice update reports.
Automated workflows are particularly useful to reduce your admin time and to keep engaging with your clients at regular touch points. With Quenza, for instance, you can also create pathways which are tailored sequences or exercises or worksheets for in between sessions.

Finally, you also want a client engagement platform that allows you to integrate other tools as well as scale up your business. One example is that Quenza has group therapy or group coaching features which is a powerful way to expand your reach.
In short, the world has moved on significantly since traditional customer relationship management (CRM) tools. These were more of a process tracker for sales than the versatile and insightful systems we have today. The table below gives you more details as to what else you can expect from a client engagement tool software.
| Features | Traditional CRM System | Client Engagement Tool |
|---|---|---|
| Scope and focus | A CRM is usually run on business servers to track sales leads, pipelines and anything to do with the funnel. | Client engagement systems focus on engagement rather than just management. They’re often cloud based and track preferences and behaviors rather than just touch points from sales teams. |
| User interaction | Commonly used CRMs tend to simply track when and what was bought. | With a broader focus, a client engagement platform might use artificial intelligence and collate interactions on social media and websites to provide unique customer and client insights. |
| Functionality and features | With a CRM, the focus is transactional and as such, sales activities are tracked. | Client engagement applications are more flexible and are more client-facing. Clients can find themselves on the same portals that enhance their overall experience. This is particularly true in a service role like therapy or coaching. |
| Predictive capabilities | CRMs are not normally connected to any other systems, including AI. They simply track the data that is input into them by the sales or business teams. | As engagement platforms are connected to a range of systems, including AI and machine learning, they can give more relevant client insights. |
| Integration capabilities | There are limited integration options with traditional CRMs. | Client engagement software is specifically designed around digitally-minded clients. They therefore integrate with all major platforms including social media, instant messaging and other digital or third-party platforms. |
Chapter 3
A Look at Client Engagement Systems
If you’re reading this, you’ll already know that you have a wide choice when it comes to working with the right client engagement platform. The final decision is a mix of logic and intuition.
The challenge is that intuition only really works if you have years of experience to help you spot patterns, almost subconsciously[3]. So, most of us have to rely on user reviews and overall presence.
Having said that, most platforms offer a trial for you to test things out. A great way to start engaging your clients early is to involve a select few in the trial and get their feedback.
Nothing in this world is perfect and we all have to work out the right balance between pros and cons for our needs. Below is a table showing some of the top platforms out there to get you started on what to look for.
| Platform | Strengths | Limitations |
|---|---|---|
| Hubspot | An all-in-one platform that brings together marketing and sales through an intuitive dashboard that easily integrates with other systems. | It has a complicated pricing system which can increase costs quite quickly. |
| Pipedrive | A sales-focused CRM that can be extended to boost client engagement. Provides proactive and visual sales pipeline management tools with customizable features. Good integration with other tools. | Advanced reporting needs special plug-ins. |
| Intercom | As one of the first engagement platforms, Intercom prioritizes conversational engagement with clients with multiple touch points throughout the sales journey. | It has limited reporting features. |
| Freshdesk | A collaboration engagement software that is designed for collaboration with other teams and customers. | Some features, such as the workflow automation, can be costly. |
| Quenza | An all-in-one platform that offers you automation so you can spend more time with clients as well as client dashboards to provide an experiential journey. Quenza has everything from activity builders, communication features, automated reminders, documentation, storage, goal tracking, business analytics and even client Engagement tool notes software. | You’ll need to integrate a separate video conference platform if you do remote sessions. |
Chapter 4
The Power of a Client Engagement Tool
The best engaging clients software allows you to follow the whole journey of the key stages of client engagement. As you can imagine, the aim is to create an emotional attachment during that journey. This can include anything from creating online brand communities to using blogs, podcasts, user generated content and more[4].
The more you get that right, the more likely those same people will become advocates for your services.
Whilst the tools to engage clients have evolved with technology, the theories and frameworks haven’t changed much over the past 10 years or so. As such, it’s helpful to keep the Customer Engagement Cycle in mind.
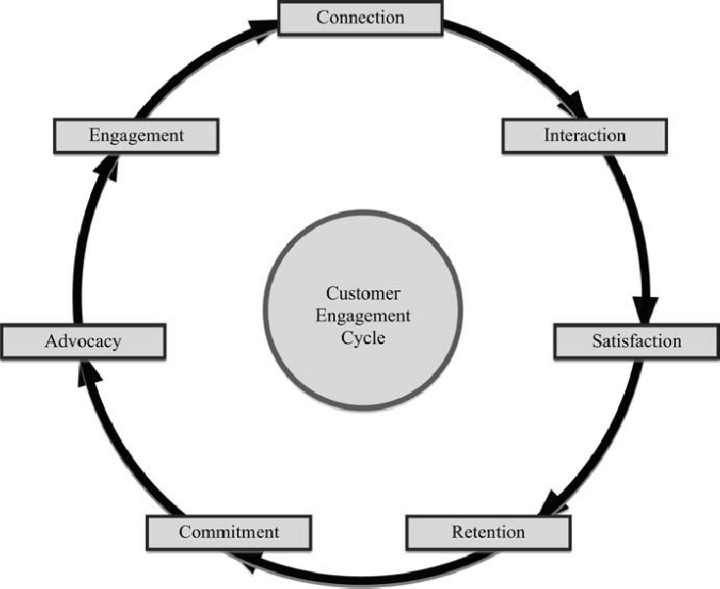
Customer Engagement Cycle[5]
For each stage, your goal is to use a client engagement solution that shows your skills, uniqueness and style. For example, you could connect through social media, interact through instant messaging and show how your approach can satisfy their needs.
Retention relies on offering an exceptional service whilst building commitment through trust and experiential interactions.
Self-Compassionate Goal Pursuit
For instance, with Quenza you can easily send premade exercises or worksheets to your clients in between sessions to keep their goals in mind. As an example, this one takes clients through how to practice self-compassionate goal pursuit. They are then more motivated and passionate about their whole experience and journey in general.
The key when working with a client engagement tool platform is to keep an eye on the big picture. Clients can become your advocates now or in the future as you never know when they might refer someone to you. Consequently, keep checking in with them and following up with new discoveries from the field or other relevant content for them.
Finally, our table below summarizes what you can expect to gain when working with the right software.
Benefits of Client Engagement Platform
| Benefits | Description |
|---|---|
| Engender loyalty | For instance, you can set up special membership access to resources on your website, based on what you know about what interests your clients. |
| Faster troubleshooting | With intelligent chatbots, questions and issues can be answered at any time, even when you’re asleep. |
| Personalized website experience | Use the data from your engagement platform to create dynamic content for the right people in your niche. |
| Value based relationships | As you get deep insights into your clients’ preferences, habits and issues, you can check in with them by sending tailored content or refresher exercises. |
| Secure storage | Taking notes and documenting therapy or coaching sessions is critical for you as a practitioner so you can keep building on progress. With client engagement tool notes software, creating and filing those notes has never been so easy or efficient. |
Chapter 5
Mobile Client Engagement
You might already instinctively know that mobile apps create a stronger and better relationship with customers so building deeper engagement. While every business needs an online presence, mobile apps remain your most strategic asset[6].
The research further shows that mobile apps are convenient touch points that can correlate with location and real-time problem-solving. For instance, QR codes are now common features.
Although, it’s worth remembering that the quality of your client relationships remains the single most important driver of customer loyalty, again, according to the research[6]. Therefore, your goal is to tailor whatever client engagement tool program you use, regardless of whether it’s an app or web application, for your specific clients’ needs.
In order to then build the best possible relationships you can, it’s worth noting what both options can give you, as summarized in the table below.
Leveraging the Benefits of Mobile Apps versus Web-Based Applications
| Mobile Apps | Web-based Applications | |
|---|---|---|
| Platform | Client engagement apps use software specifically designed to be accessed on mobile phones whether Android or iOS. | Usually, software built to be used on computers or laptops. |
| Features | User-centric design with a smooth and intuitive experience including, for example, touchscreens. | Client engagement applications often have more extensive features because of greater processing power and larger screens. |
| Data storage | Client engagement tool apps can often work offline by storing data locally and then syncing once they’re connected to the web again. | Often used for data-intensive operations that might need data analysis or visualization. Dat is then often stored in centralized servers. |
Chapter 6
Engaging Clients in the Digital Age
A client engagement platform can revolutionize your business, no matter what it is. This is even more relevant for therapists or coaches whose very existence depends on getting to know their clients at a deeper level.
On the one hand, your client engagement tool solution provides you with the technology you need to be more effective. You’ll have a consolidated dashboard with all the data you deem relevant to manage your business. All workflows can then be automated from there according to your unique needs.
Alongside engagement metrics, trends and improvement areas, you’ll also be able to deep dive into clients and their individual progress. With Quenza, for example, you can then decide to further engage with one of those clients by sending out a new exercise or worksheet, particularly if they’ve just met with a roadblock.
Strengths During and After Challenging Times
In this exercise that you’ll find in Quenza’s vast library of client worksheets and exercises, clients work through reframing a problem from a strengths viewpoint. They can work through it on their phone or computer so as client engagement tool apps go, this one is versatile.
Aside from automated workflows and interactive dashboards, client engagement systems give your clients features that they now expect as part of the norm. With the right platform, your clients will feel just as empowered as you in their journey collaborating with you.
Summarizing How Engagement Platforms are Impacting Client Interactions
Real-time response
- Client engagement tool applications enable clients to get their questions answered instantly. With today’s software, platforms can do some client engagement tasks outside your working hours.
AI Personalized
- Thanks to AI, that engagement is highly tailored and is already starting to build trust and a connection with potential clients.
Multichannel Engagement
- A good client engagement tool seamlessly integrates across multiple digital channels including social media, chat, email and SMS at any time.
Data-Driven Insights
- With the right client engagement platform, you get insights about your clients so that you can tailor your communication according to their needs.
Chapter 7
Defining Success
All business owners are also clients and customers for someone. Think about how much the right digital interaction makes a difference to how you feel about the business? In other words, what do your favorite businesses do that feels right in terms of engaging clients software?
Similarly for your clients. Whether you’re trying to increase your generated leads, geographic presence, client loyalty or operational efficiency, people need you. You actually do a disservice to those who need guidance and support but don’t know how to find you.
Instead of letting your ideal customers suffer needlessly, get the right client engagement platform to discover who needs your support and guidance and how to connect with them. Whether you’re a coach or therapist, people throughout the world have never needed help more than today.
Another way to think about it is to consider what happens if you don’t use an engaging clients platform? In short, you’re not working to your potential and you leave disappointed people behind you.
The Risk of Not Working with a Client Engagement Platform
| Risks | Overview |
|---|---|
| No Shows | Therapy and coaching mean hard work for both parties but without engagement, clients can simply revert to old habits. Instead, with the right platform, you can encourage and motivate them seamlessly throughout the journey. |
| Stuck clients | Sometimes clients are just stuck and need our help. At other times, they get overwhelmed by clunky processes and too much paperwork. Make sure that doesn’t happen to you by choosing a platform that can automate your filing, invoicing and messaging where appropriate. |
| Lost time | How many hours have you wasted sending out invoices or looking for documents? A client engagement platform takes all that away through automation and secure filing. |
| “Wrong” clients | The most successful therapists and coaches know their niche. They know how to market themselves, including with the right therapy or coaching bio, to the people they know they work well with. As a result, they don’t lose time with mismatched clients or send out disgruntled and confused people simply because they didn’t gather the proper data. |
Chapter 8
Choosing the Right Client Engagement Tool
Blending intuition and logic isn’t always easy especially when faced with so much choice. A more practical way to start choosing your client engagement platform is by listing your needs based on the features you should look for.
We’ve summarized the top factors you to review when reviewing client engagement tool systems in the table below. As you read through them, remember that the platform needs to work for you. As a result, you might have a preference for the level of customization available.
Most importantly, you’ll need to make sure that your client engagement platform can scale up to whatever your vision is set to. Then, it’s a balance of cost versus impact.
Last but not least, you might also want to explore how a vendor might partner or collaborate with you to support your growth strategy. In essence, you’ll want to understand how they support clients and keep their own systems up to date with technical advancements.
By giving trials a go, you’ll get a feel for what’s possible and how to take your clients’ experience to the next level. Best of all, Quenza’s guarantees all the key factors as detailed in the table below.
Key Factors to Review when Choosing a Client Engagement Platform
| Factors | Overview |
|---|---|
| Simplicity and experience | First and foremost, you must feel comfortable and at ease using your client engagement platform. Moreover, make sure it provides the type of experience that both you and your clients expect. |
| Scalability | It’s important to verify that your platform of choice can grow with your business. |
| Integration and flexibility | You need a system that can incorporate platforms you’re already using whether it’s social media or a scheduling tool. |
| Customization | You’ll want to make things your own so choose a tool that allows you to change its dashboards and processes to fit your business. |
| Security and compliance | Most critically, check that your chosen platform is both HIPAA and GDPR compliant so that you don’t have to worry about privacy and security. |
Conclusion
With everyone facing increasing complexity and uncertainty in their lives, people want to be connected to the businesses they buy from. They want to do the right thing and to belong to a community. With client engagement apps, you have the opportunity to create that community that your clients crave.
Yes, a client engagement platform gives you the data you need to reach your ideal client but it also gives you the chance to add your human touch. With the right information, you can nurture deeper relationships and make more of a difference in this world. You’ll help more people than before and as an added bonus, your business will grow.
Quenza is unique in its quest to make an impact on the world because it too blends technology with the human touch. Its all-in-one client engagement platform offers everything you’d expect including automated workflows, interactive dashboards, client portals and messaging suffers.
Moreover, it has a vast library with over 200 exercises, worksheets, metaphors, meditations and much more that allow you to build those perfect experiential client journeys. All of the resources are from science-backed psychology therapies and they’ll impress you with their simplicity and effectiveness.
Why not see for yourself by signing up for the full-access, free trial for one whole month? Your clients will feel more supported than ever before.
Frequently Asked Questions
Essentially, it’s a software program that allows you to manage your client relationships. It gives you data and insights about their behaviors, issues, buying habits and preferences. From there, you can be more strategic in how to target your ideal client and then build a strong level of loyalty.
In short, apps are for mobile phones and applications tend to be web-based for computers or laptops. As a result, apps tend to work well in real-time but applications have more features and tools because they have greater processing power.
You’ll need something that’s both easy to use but also compatible with your current systems and business workflow. Most importantly, make sure it’s secure and HIPAA and/or GDPR compliant.
A client engagement platform is critical in today’s digital world because clients are tech-savvy and they know what they want. You therefore have to tailor your approach to make them feel that they are your only client. The only way to do that effectively is through a client engagement platform. You won’t regret it when you find yourself supporting more people than ever.
References
- ^ Team, M. D. 3. (2023, June 1). Microsoft and Futurum research: Discover insights to create experiences that customers love. Microsoft Dynamics 365 Blog. https://cloudblogs.microsoft.com/dynamics365/bdm/2022/12/08/the-key-to-delivering-experiences-that-customers-love/.
- ^ 15 Eye-Opening Corporate Social Responsibility Statistics. (2021, June 15). Business Insights Blog. https://online.hbs.edu/blog/post/corporate-social-responsibility-statistics.
- ^ Kutsch, L. (2019, August 14). Can we rely on our intuition? Scientific American. https://www.scientificamerican.com/article/can-we-rely-on-our-intuition/.
- ^ Bansal, R. (2016). CUSTOMER ENGAGEMENT – A LITERATURE REVIEW. ResearchGate. https://www.researchgate.net/publication/318224473_CUSTOMER_ENGAGEMENT_-_A_LITERATURE_REVIEW.
- ^ Sashi, C. (2012). Customer engagement, buyer‐seller relationships, and social media. Management Decision, 50(2), 253–272. https://doi.org/10.1108/00251741211203551.
- ^ Khan, I., Hollebeek, L. D., Fatma, M., Islam, J. U., Rather, R. A., Shahid, S., & Sigurðsson, V. (2022). Mobile app vs. desktop browser platforms: the relationships among customer engagement, experience, relationship quality and loyalty intention. Journal of Marketing Management, 39(3–4), 275–297. https://doi.org/10.1080/0267257x.2022.2106290.
