Each day, technology continues to change the face of healthcare, helping providers deliver better quality healthcare to their patients. With more and more patients visiting healthcare facilities every day, the role of digital innovations is especially apparent in the growth of e-clinics, and e-clinic software.[1]
But with so many remotely located patients, how do virtual care practitioners in e-clinics stay organized, while nurturing customer relationships and ensuring consistent, high-quality care?
In this article, we’ll look inside a typical e-clinic, looking at some of the e-clinic software that helps providers streamline their office manage, while marketing, spending quality client time, and growing their businesses.
Before you read on further, we recommend you sign up for our Quenza trial, which will give you unlimited access to all of its specialized health features for free. Our HIPAA-compliant e-clinic solution will give you all the tools you need to create individualized treatment plans, streamline your documentation, and deliver a professional, positive patient experience that changes their lives for the better.
What is E-Clinic Software? Key Features
How does e-clinic software differ from therapy software, or a client relationship management (CRM) system?
Broadly, e-clinic software systems cover a huge array of various services and features, all of which are designed to help manage hospitals and clinics efficiently.
In other words:
E-Clinic software describes the digitally automated systems that are designed to store and track patient data, as well as streamline the day-to-day processes of hospitals and clinics.
By incorporating patient services, and practice management features, the right system can help providers to better deliver core mental health and healthcare services, while automating routine, administrative tasks.
Providing Patient Services
First, many software solutions add value by providing many services directly to patients, for example, through:
- Digital appointment, reminder, and scheduling functions
- Automated client billing and invoicing
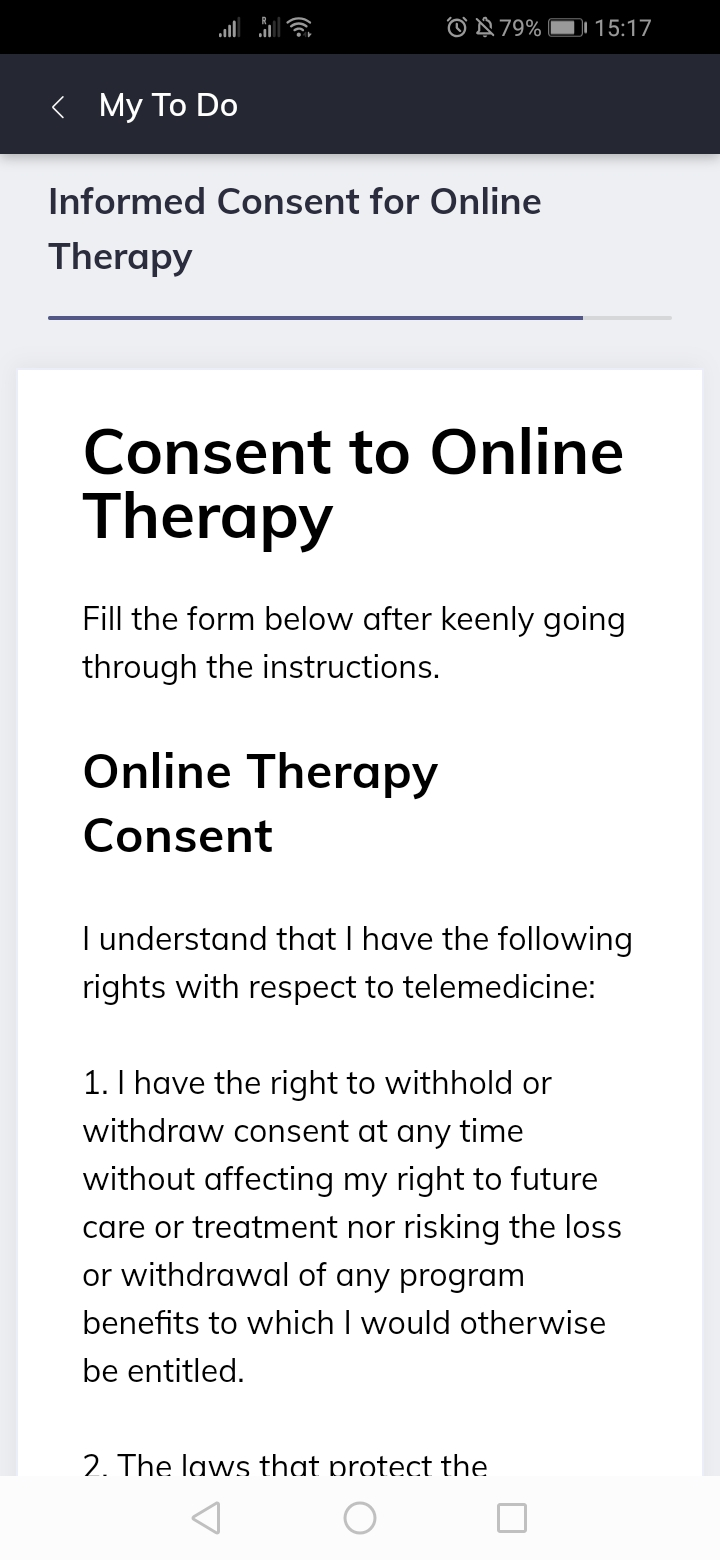
- Digital registration and forms, such as Informed Consent
- Patient medical records, such as Therapy Intake Forms, and more.
Designed primarily to save time on non-essential tasks, they allow telemedicine providers to focus more on virtual sessions, online treatment plan creation, personalization, and other core healthcare services.

Care pathway automation tools and ready-made treatment plan templates are just two examples of how e-clinic software
Improving Practice Management
On the practitioner side, e-clinic software is often packed with inbuilt practice management features for enhanced office management, saving admin, patient, and practitioner time.
Often, it provides access to important insights central to patient care, integrating with Electronic Medical Records (EMR) and nutrition software or medical databases.
Many types of data can be stored on e-clinic software, including:
- Diagnoses
- Prescriptions
- Hospital visits
- Payment and contact details, and
- Appointments.
In the table below, you’ll find some of the most common practice management features found in e-clinic software today:
|
Function |
Benefit |
|---|---|
|
Reporting |
|
|
Billing |
|
|
Marketing |
|
|
Scheduling |
|
|
Charting and Record-Keeping |
|
|
Finances |
|
At a Glance
By combining patient-facing functionalities with practice management capabilities, e-clinic software solutions monitor and track the day-to-day operations of a healthcare institution, streamlining activities, and enriching the way that patients experience their general or mental healthcare.
The next sections take a closer look at these different features of e-clinic software so that you as a provider can decide what features you’re looking for in your ideal solution.
E-clinic software solutions monitor and track the day-to-day operations of a healthcare institution, streamlining activities and enriching the way that patients experience their general or mental healthcare.
Reporting
Many e-clinic software suites can be used to consolidate and better process patient and staff data, for a more organized approach to practice management.
Reports from Patient Data
Electronic Medical Record (EMR) systems are fairly widespread in healthcare today, as a more eco-friendly, convenient, and organized way to manage patient health records. An essential feature in e-clinics, EMRs help keep vital patient information confidential while allowing for easy practitioner access.
Through EMR functionalities, e-clinic software suites can speed up reporting processes by pre-populating fields from patient data. Whether you’re working as an occupational, physical, or speech therapist, this enables quicker and easier overviews based on:
- Activity and fitness statistics
- Treatment histories
- Medical histories
- Previous provider data, and more.
With most reporting features, care providers can also view daily patient visits, where they came from, who they have seen in the hospital, and how much has been charged. Such reports will help your institutions to stay on top of the business.
Human Resource Management
Using e-clinic software, hospital management can also calculate key financial statistics, such as the most profitable treatments and care providers. HR features often also simplify compensation and remuneration for staff.
Complicated data analysis is further simplified by charting and graphing capabilities, based on reports, and which can be further grouped into relevant categories such as clinic, marketing source, or practitioner.
As well as this:
- E-Clinic software can even be integrated with other reporting software solutions, allowing practitioners to easily generate good-looking custom reports for clients
- Often, hospitals and clinics can submit reports directly from the software – useful for lodging insurance reimbursement claims, and
- e-clinic administration can easily generate reports on details of monthly or annual clinic expenses.
Billing with e-clinic Software
The most common billing and invoicing options offered by e-clinic software allow users to invoice patients, insurance companies, and other relevant stakeholders. Frequently, it’s possible to send invoices digitally in a way that can later be tracked.
Inventory and Payments
Billing functionalities also simplify payment and inventory processes such as:
- Setting up consultation, treatment, and product price lists – when a system allows users to enter barcodes, this is also handy for inventory management, alerting users when stock runs low and keeping track of packages and deliveries
- Enabling users to apply discounts, make and receive payments using a variety of methods
- Automating and standardizing patient and supplier billing
- Sending automated payment reminders – as well as creating promotions, custom orders, and discounts for clients
Revenue Cycle Management
Most e-Clinic software systems come with built-in billing modules to help reduce the stress of revenue cycle management. These billing features help manage patient accounts by keeping a list of all previous and present payment data and diagnoses.
When patients check in, more comprehensive e-clinic billing modules may also confirm insurance eligibility, ensuring everyone gives consent about copays and deductibles.
Finally, it’s possible to find e-Clinic software solutions that create reports on financial transactions. This makes it easier to calculate and process your institution’s profits and employee commissions.
Marketing
But can you use e-clinic software to grow your practice?
The short answer is yes – as many digital clinical solutions are designed by practitioners with healthcare experience, we’re seeing more consumer-focused systems that cater to all provider needs.
Among these features, marketing capabilities that allow you to target key groups and reach new clients, while engaging patients and customizing your communications.
Many e-clinic software solutions include marketing capabilities that allow you to target key groups and reach new clients, while engaging patients and customizing your communications.
Marketing Communications
With some e-clinic software, practitioners can now target specific patient or prospective client groups with relevant marketing messages.
For example:
- Patients who make inquiries, but don’t book an appointment
- Reaching out to past patients with similar products or treatments
- Selecting key demographics in the area with new offers, treatments, or services.
Customized Correspondence
Using email, postal templates, or text messages, e-clinic software can usually be customized so practitioners can send branded, professional-looking correspondence.
Simultaneously, it often supports bulk mailing by integrating with online marketing services, such as Mailchimp.
For larger healthcare institutions, it may be worth looking into specific services such as direct website integration or outbound call management, while smaller practices may prefer a simpler, more affordable option.
Scheduling Using E Clinic Software
Gone are the days of phone call appointments – with modern E-Clinic software scheduling modules, patients can now easily make appointments themselves, online.
Patient Portals
Most online patient portals are easy for clients to use. Pre-built into many treatment software systems, they may allow patients can book, reschedule, or cancel appointments to free up practice desk staff.

Patient portals are also used to securely and privately share practice documents such as intake forms and informed consent agreements, or e-health interventions. On HIPAA-compliant platforms like Quenza above, patient responses and data are confidentially stored and sent to the practitioner to use in treatment planning, case reviews, and more.
Scheduling
When patients make an appointment, the e-clinic software may also send automated reminders via text message, email, or phone, reminding them about the appointment and minimizing the risk of no-shows.
E-clinic scheduling features may also:
- Store information about previous visits, including previous patient no-shows
- Be equipped with intake documentation, informed consent forms, and more, which patients can fill out at home, and
- Estimate how much time visits will take, based on this data.
Practitioners can then manage schedules more easily, for smoother operations and more quality patient time.
Storing E-Clinic Medical Records
Medical record-keeping, another key healthcare process, ensures that providers can store, monitor, and access patient medical records digitally.
When it comes to blended care solutions, some e-clinic software comes equipped with its own charting modules, while other suites may integrate well with independent Electronic Health Record (EHR) software solutions.[2] In general, most also offer record-keeping functionalities to facilitate better office management.
Charting Capabilities
Charting features allow practitioners to more easily record, update, and store important patient information safely in a digital system – often securing it through encryption, and enabling speedier access in the future.
Many systems also create patient flowcharts, recording immunization, diagnoses, prescription details, and other e-health information.
Record-Keeping Features
Typical record-keeping modules include several features that practitioners can use to customize their experience, enabling them to access or refer to:
- Patient history
- Patient referral trackers
- Clinical charting
- Transcription options, and
- Lab orders and results, to name a few.
While you may not require all, the right software for your practice will ideally be available from numerous remote locations, giving you better access to important patient data from practice forms, surveys, or assessments when and where you need it.
Financial Dashboard
Monitoring and tracking your clinic’s finances is also important, and a financial dashboard allows e-clinic administrators to analyze and improve the institution’s performance.
Financial Decision-Making
Financial dashboards in e-clinic software let administrative staff know a wide variety of things to make better decisions.
For instance:
- The organization’s overall financial health – including revenue metrics, patient flow, lost income from canceled appointments, and the reason for cancelation or rescheduling.
- Areas that need improvement for a better patient experience, and
- Revenue generated – often, by doctor, department, or specialty
In short, a user-friendly financial dashboard will monitor the financial performance of the organization, while giving insights into how practitioners can improve their clinic.
When analyzing the data and metrics in a user-friendly format, administrators can make decisions on how to increase profits – such as by expanding the most lucrative departments in the institution.
Common Questions about E-Clinic Software
Unfamiliarity is one of the main reasons some practitioners still hesitate to adopt new telehealth platforms.[3]
Here, we answer some of the most common questions about e-clinic software today.
|
FAQ |
Details |
|---|---|
|
How will my hospital benefit by adopting e-clinic software? | E-clinic software offers many advantages to healthcare institutions that integrate it to their systems.These systems help institutions increase revenue while cutting expenses, streamlining day to day operations, facilitating quality and timely healthcare, good data organization, and minimizing documentation errors.
E-clinic software systems enable a clinic to perform at its best. |
|
Can I get support for e-clinic software? Where? | In general, yes.Most software service providers offer 24-hour support once you purchase their products.
In most cases, vendors have teams on standby to answer technical questions and help you solve issues. Further, as some institutions may want out-of-hour support, it’s not too hard to find service providers offering round-the-clock cover for an additional cost. |
|
How much does it cost to integrate and run? | The initial cost of integrating e-clinic software will vary according to the service provider and your needs.For instance, there types of software that are general and while others are carrying out specific functions, such as blood testing or inpatient tracking.
You might also require training after installation – all factors which mean the cost of setting up the system can vary. |
Enhancing Patient Engagement through E-Clinic Portals
E-clinic software is revolutionizing patient engagement through comprehensive patient portals. These digital interfaces serve as a bridge between healthcare providers and patients, offering a range of features that empower patients to actively manage their health while streamlining communication with their healthcare team.
Patient portals typically provide secure access to personal health information, including medical history, test results, and current medications. This transparency lets patients stay informed about their health status and treatment progress. Many portals also offer educational resources tailored to patients’ specific conditions, helping them better understand their health and make informed decisions.
Appointment management is another key feature of patient portals. Patients can easily schedule, reschedule, or cancel appointments, reducing no-shows and improving clinic efficiency. Some advanced portals even offer AI-powered chatbots that can handle basic inquiries and guide patients through scheduling, freeing up staff time for more complex tasks.
Many e-clinic patient portals now include features for tracking personal health goals and logging health-related data. This might include diet and exercise logs, symptom trackers, or medication adherence tools. By engaging patients in their health management, these features can lead to better health outcomes and increased patient satisfaction.
Final Thoughts
As blended care plays an ever-widening role in the way we deliver healthcare, e-Clinic software is playing a pivotal role. From standardizing systems to sustaining top performance, they’re now easier than ever to introduce to your practice – whatever the size.
If you’re looking to ensure smoother healthcare or therapy services in your niche, minimize redundancies and errors, and cut down patient wait time significantly, there are plenty of affordable options that can be customized to your unique requirements.
Do you have any experience with e-clinic software, either as a patient or as a provider? Please do share your story below in a comment.
We hope you enjoyed our article. To start delivering gold standard blended care solutions in your e-clinic, check out our free Quenza trial. Our telehealth software for coaches, therapists, and psychologists will help you deliver tailored, professional e-health solutions online so that you can enhance the well-being of your patients even more effectively.
References
- ^ Drake, T. M., & Ritchie, J. E. (2016). The surgeon will skype you now: advancements in e-clinic. Annals of Surgery, 263(4), 636.
- ^ Institute of Medicine. (2003). Key capabilities of an electronic health record system. Retrieved from
- ^ Deloitte. (2018). Virtual health: Extending the human touch in care delivery - Strategies to engage physicians and encourage adoption. Retrieved from https://www2.deloitte.com/content/dam/Deloitte/us/Documents/life-sciences-health-care/us-lshc-virtual-health-care-physcian-adoption.pdf

