Thoughts and observations tend to quickly get distorted after any discussion. Moreover, therapists, counselors, clinicians, and coaches can get called upon to refer to past sessions for various reasons. What better way to organize your thoughts than with some DAP notes?
The DAP structure is a standard format for creating clear, informative notes efficiently. If you’re an online counselor, healthcare provider, coach, or therapist looking for an organized framework, this guide shows you how to create your own brilliant DAP notes templates with a solid structure and format.
What are DAP Notes in Counseling?
The DAP format offers an organized and efficient structure for practitioners to create progress notes, psychotherapy notes, and other practice documents. In short, it’s a useful note-taking framework for counselors, psychologists, and other healthcare providers to track their clients’ progress.
It’s worth noting that DAP notes, just like progress notes, are documents that can be shared with other healthcare workers, as per the HIPAA privacy and sharing rules.
On the other hand, psychotherapy notes tend to be for a practitioner’s private use only. Although, these can be subject to some legal exceptions such as in abuse cases.
DAP stands for the various sections that constitute a counseling note:
- Data
- Assessment, and
- Plan.
In mental health contexts, the DARP acronym is occasionally used instead. Here, the “R” represents an additional “Response” section, where a counselor records a client’s response to the described assessment.
What To Include in DAP Notes
Each section, as detailed below, provides a handy framework to record all the key details of a session:[1]
- The Data heading covers everything that occurred during a counseling session, effectively combining both the objective and the subjective information received. This includes, but is not limited to, a client’s observable responses, affect, traits, and behavior. Overall, the practitioner records all the specific information about what was said and observed.
- Under Assessment, counselors interpret and analyze the data in the previous session resulting in clinical hypotheses and diagnoses while incorporating all the information noted in the data section above. While they apply some professional subjectivity, counselors note how each session supports the client’s overall treatment goals as well as the client’s response and any potential health or self-harm risk.
- The Plan section is used for making decisions and recommending goals, actions, and timings for treatment while supporting the client’s development. Here, the objective and subjective data from the previous two sections combine to inform a counselor’s strategy or next actions – often practiced between the current session and the next. This could include recommendations or referrals for therapy and lifestyle changes, among other short- and long-term treatments.
DAP vs SOAP Therapy Notes Explained
The key difference between the SOAP and DAP formats is that the former breaks down the information about a session into two discrete sections.
The SOAP acronym is another popular therapy note framework used in mental healthcare settings, with a slightly different layout to DAP notes.
S, O, A, and P describe a patient’s session in terms of:
- Subjective data – a client’s subjective experiences, triggers, opinions, or feelings about the chief complaint (CC)
- Objective data – quantifiable data such as test results, medication, or measurements and physical diagnostics
- Assessment – a professional analysis of the subjective and objective data above, including a problem definition, and
- Plan – detailing the (recommended) next steps in a client’s treatment, including whether additional diagnostics or exploration is first required.
The key difference between the SOAP and DAP formats is that the former breaks down the information about a session into two discrete sections. This only generally applies in healthcare contexts where medications, diagnostics, blood work, and other clinical data are necessary to fully inform a patient’s treatment.
Counselors, however, don’t always need to collect ‘hard data.’ So, the single ‘Data’ heading in a DAP note covers this by consolidating all observations into one section.
DAP Progress Note Example
To give you an idea of how this works, here is one DAP Progress example of counseling session notes presented in two different formats.
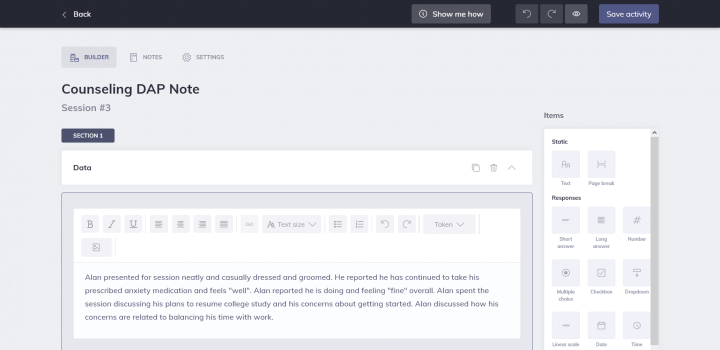
Example 1: From the 3rd session with your client Alan Ellis
Data: Alan presented for the session neatly and casually dressed and groomed. He reported he has continued to take his prescribed anxiety medication and feels “improved”.
Alan reported he is doing and feeling generally content and optimistic. He then spent the session discussing how he was energized about his plans to resume college study and hopeful, even though slightly apprehensive, that he can manage his concerns about getting started. He’s mainly nervous about being able to balance his time with work effectively but felt inspired by his recent progress in managing emotions. He wasn’t so overwhelmed this time but ready to approach the problem step by step and he skilfully described the techniques he would leverage.
Assessment: Alan engaged actively in today’s session. He presented as clear-headed and able to discuss his feelings while being optimistic about the future.
Alan was further able to identify protective factors for anxiety management as well as stress management techniques to implement if he feels panicked. Alan also identified two other people he can call for support to assist with resuming his studies and when his mood drops.
Plan: Next appointment is 11/26/22 @ 9:00 AM.
In the above graphic, you can see the same notes in an online format using therapy notes software Quenza. This software makes it very simple to create DAP templates to suit your style thanks to the intuitive text boxes and sections from Quenza’s Activity builder.
Once complete, you can then access your templates whenever you want to write therapy notes.
DAP Notes Assessment: A More Detailed Example
Knowing what to state in the Assessment section of DAP notes can be a little tricky for newcomers. Nevertheless, the overarching goal is to offer your clinical interpretation of the data.
Here, you’ll answer key questions such as:[2]
- According to the data, how is my client trying to address their challenge?
- What progress are they making?
- After reviewing the data, what is your preliminary diagnosis?
- What working hypotheses can be drawn from this session?
- What is the root cause of the chief complaint?
Another assessment notes example might look as follows:
“John continues to experience a mild depressive episode and is unsure about continuing with his psychiatrist. He had difficulty coming up with ideas for an action plan when I noted his goal from the last session. Nevertheless, he showed engagement in brainstorming strategies for finding a more creative job while simultaneously embracing his emotions.”
How To Write DAP Case Notes: 7 Tips
DAP notes are simple to write with the correct digital templates – here are our tips on formatting the perfect note and recording group sessions in Quenza.
How To Format DAP Notes
To create your first DAP note template, all you need is a blank template in Quenza’s easy-to-use Activity Builder:
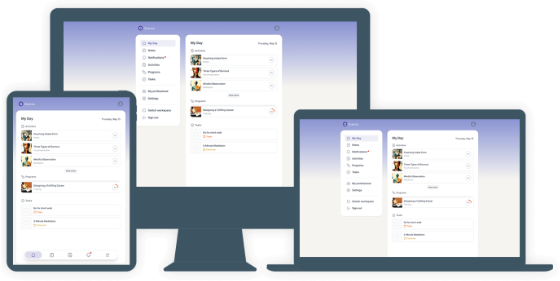
Here in your Activity builder, you can create and title various sections for each of your Data, Assessment, and Plan headers, plus any additional sections you find helpful.
When you’re done, simply save your DAP note template. You’re now ready to open a copy for each session you’d like to record!
Once you’ve got the hang of it, try out these formatting tips to take your notes to the next level:
- Play around with custom sub-sections if you feel that might be helpful – you can always edit your templates if you think of ways to improve them
- Upload your practice logo to your DAP note templates using Quenza’s White Label feature
- If you use a voice recorder, upload your mp3 files to complete your DAP notes
- Combine text with check boxes, drop-down menus, or sliding scales for faster note-taking, and of course,
- Keep it clean, simple, and relevant when you’re documenting your sessions.
Accessing Group DAP Notes
Creating DAP notes for any coaching or therapy groups you work with is just as simple.
You can easily follow the same steps to create helpful group templates as we’ve just seen. Alternatively, you might want to use the DAP structure in Quenza’s Client Group Notes to store them securely by group:

Creating Client Notes for each group not only keeps them in chronological order but also stores them privately so that they are visible only to you – the counselor.
Here, you might want to:
- Download your notes as PDFs for your files, or
- Time-stamp and date your DAP therapy, psychology, or counseling notes so you can easily access your notes from specific sessions in a flash.
3 Helpful Templates For Your Sessions
If you’re looking for a few DAP note templates to help you start, some of the following might interest you:
- This downloadable DAP note walkthrough from Rutgers University provides a few pointers to help you create succinct, but informative notes
- Sample Templates provides a few free DAP mental health progress notes examples and templates, and
- The Area Substance Abuse Council offers an example template that may be useful.
Best Online Solution For Writing DAP Notes
The most efficient, effective way to create DAP notes as a mental healthcare provider is to use specialized software, more specifically, HIPAA-compliant software.
Unlike downloadable documents and other files, therapy notes software is specially designed so that you can reuse your templates repeatedly. You then know that everything is stored safely, securely and privately as per industry requirements.
DAP note templates are quick, stress-free, and very simple to create using Quenza. Not only can this save you a great deal of time but it also keeps you organized.
Designed especially for therapists, Quenza is unique in allowing you to tailor, refine, and modify your templates whenever you like. Furthermore, with Quenza, you have a HIPAA- and GDPR-compliant platform that also enables you to:
7 Unique Features And Tools in Quenza
If you’re a general or mental healthcare professional, there are more than a few ways Quenza can help you in addition to writing clear, accurate DAP notes efficiently.
Some of the unique Quenza features that you can use to run your practice, grow your business, and help others include:
- A Wheel of Life tool. A simple-to-use therapy or coaching tool for creating unique self-assessments
- The Wheel of Emotions. Use the Activity Builder Wheel of Life tool to create this effective intervention so that your clients can learn to connect to emotions by naming them. For instance, Alan, in our example above, could have found this particularly useful.
- Quenza Chat. Real-time, HIPAA-compliant client chat through your mobile or browser
- A Group Coaching or Therapy feature. Run workshops, programs, or e-courses with up to 50 participants at once
- A free multilingual client app. Helping you deliver a more personalized coaching or therapy experience in 16+ languages
- Custom emails. So you can email clients from your private practice email address, and
- Custom brand colors. Helping you promote your business by creating a coaching or patient portal in your own brand colors!
Incorporating DAP Notes into Your Workflow
To fully leverage the benefits of DAP notes, it is crucial to integrate them seamlessly into your daily workflow. This involves setting up a consistent routine for note-taking that ensures every session with a client is documented accurately and promptly. Practitioners should start by creating a structured template that includes all essential components of DAP notes: Data, Assessment, and Plan. By having a pre-defined structure, you can ensure that all necessary information is captured systematically.
Additionally, it is beneficial to familiarize yourself with digital tools that can simplify this process. Software applications like Quenza not only provide customizable templates but also offer features such as automated reminders, secure storage, and easy sharing options. Integrating these tools into your practice can save time and reduce the likelihood of errors. Furthermore, developing a habit of reviewing and updating notes immediately after sessions can enhance accuracy and provide more detailed records, which are invaluable for tracking client progress and planning future sessions.
Benefits of Digital DAP Note-Taking
The shift towards digital note-taking has revolutionized the way healthcare providers manage their documentation. Digital DAP notes offer numerous advantages over traditional paper-based methods. Firstly, they enhance accessibility; practitioners can easily retrieve and review notes from any device, whether they are in the office, at home, or on the go. This flexibility is especially beneficial for those who manage a large caseload or work in multiple locations.
Moreover, digital notes improve collaboration among healthcare teams. With the appropriate permissions, notes can be securely shared with colleagues, allowing for coordinated care and better outcomes for clients. Digital tools also often come with features such as spell check, auto-save, and cloud storage, which reduce the risk of losing important information and ensure that records are always up-to-date. Furthermore, the use of encryption and secure platforms ensures that sensitive information remains confidential, complying with regulations like HIPAA.
In addition to these practical benefits, digital note-taking can also contribute to more efficient billing processes. By maintaining clear and organized records, practitioners can provide accurate documentation to insurance companies, reducing the time and effort required to process claims. Overall, the adoption of digital DAP notes represents a significant advancement in the field of healthcare documentation, providing a robust solution that enhances both efficiency and quality of care.
Final Thoughts
DAP notes can clear up a lot of confusion for mental healthcare providers, especially those in sectors where objective data doesn’t play a large part in a patient’s treatment.
If you regularly make session notes but still don’t have a set format, it’s worth creating a DAP template of your own. It may just help you write noticeably clearer and more helpful documentation.
We hope you enjoyed reading this guide. Don’t forget to begin your free 30-day Quenza trial.
With unlimited access to Quenza’s user-friendly digital tools, you’ll have everything you need to write informative and effective DAP notes easily. You’ll then be free to focus on the client solutions that drive results.
Frequently Asked Questions
DAP notes provide a more structured format compared to regular progress notes. They organize information into three distinct sections: Data, Assessment, and Plan. This structure helps ensure comprehensive documentation of each session, including objective observations, professional analysis, and future treatment strategies. Regular progress notes may vary in format and might not consistently cover all these aspects.
Yes, DAP notes are equally effective for telehealth and online counseling sessions. The format remains the same, but practitioners may need to adapt their observational skills to the digital environment. For instance, in the Data section, they might focus more on verbal cues, facial expressions visible on screen, or any technical issues that affected the session.
To ensure HIPAA compliance with digital DAP notes, practitioners should use HIPAA-compliant software like Quenza. Key practices include using strong encryption, implementing secure access controls, regularly updating software, conducting risk assessments, and training staff on privacy practices. It’s also crucial to have Business Associate Agreements (BAAs) with any third-party service providers handling patient information.
DAP notes should ideally be completed immediately after each session to ensure accuracy. However, they should also be regularly reviewed and updated as part of ongoing care. A good practice is to review notes before each new session with a client to refresh on previous discussions and track progress. Additionally, periodic comprehensive reviews (e.g., monthly or quarterly) can help identify long-term trends and inform treatment adjustments.
Yes, DAP notes can be used in legal proceedings if subpoenaed. This is why it’s crucial to maintain accurate, objective, and professional documentation. The structured nature of DAP notes can be particularly helpful in legal contexts, as it clearly outlines observations, professional assessments, and treatment plans. However, practitioners should be aware of their local laws and professional guidelines regarding the use of clinical notes in legal settings.
References
- ^ Rutgers University. Data Assessment Plan (DAP) Note. Retrieved from https://hiv.rutgers.edu/wp-content/uploads/2016/05/0000278705-DAP-Note-Form-CLEAR-wrap-up-session.doc
- ^ Theraplatform. (2020). DAP Notes. Retrieved from https://www.theraplatform.com/blog/343/dap-notes/



Very helpful 🙂