The ability to efficiently write accurate and informative case notes is recognized as an essential skill for anyone wishing to work as a therapist, coach, or healthcare professional.[1]
However, with everything that goes on in a busy practitioner’s day, it’s all too easy to fall behind on notes. Or just as problematic, spend so long with documentation that it impacts your time with clients.
The solution to these challenges is to use a progress notes template, like GIRP notes.
The GIRP framework offers a powerful communication tool by delivering a streamlined, concise, and organized account of a patient or client’s journey. GIRP notes highlight key developments and treatment plans, becoming an invaluable asset for all stakeholders.
Thanks to their structured format, GIRP documentation can be completed quickly, with minimal stress for the practitioner. This is especially the case when you use a digital care platform, like Quenza, with ready-made GIRP templates.
Keep reading to find out more. Or if you want to get started using Quenza right away, sign up for a 1-month full-access trial today.
What is a GIRP Note?
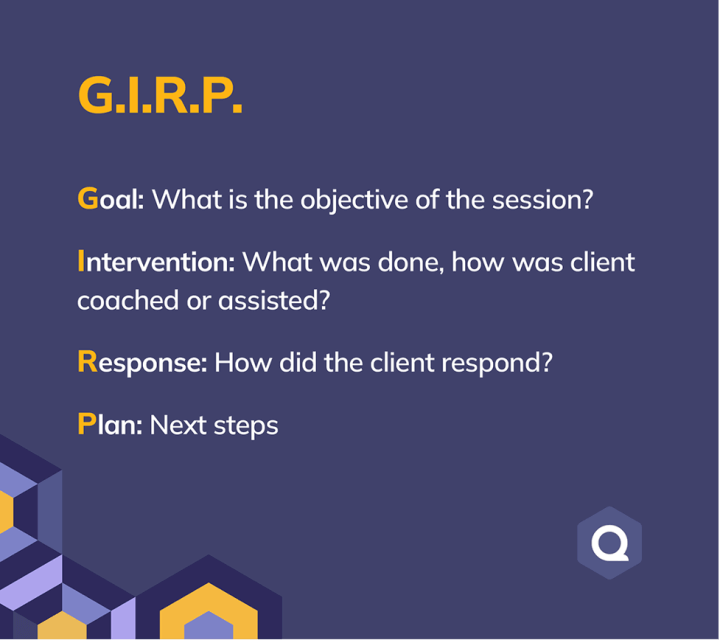
GIRP notes have earned their place as a fundamental part of healthcare and coaching documentation, offering a systematic and universally recognized method for recording patient interactions and formulating plans.
The acronym GIRP stands for: Goal, Intervention, Response, and Plan.
Goal
The unique feature of GIRP notes is that they always start with a goal.
The goal is a statement of the desired outcome or change for the individual. Or put another way, it describes what the patient wants to get out of therapy or coaching.
You might include both short and long-term goals in this first section. For example:
Janine has been attending fortnightly psychotherapy sessions to get better control of her social anxiety and agoraphobia. Long-term, she would like to have a more active social life. However, at present, her main goal is to start doing her grocery shopping in person again. Janine feels this is a safe and achievable goal for her to build some positive momentum.
Intervention
The second step in a GIRP note is to detail an intervention.
While the term “intervention” is perhaps more relevant to therapy and healthcare, that doesn’t mean GIRP notes aren’t suitable for coaching or non-clinical disciplines.
In essence, the intervention simply describes the techniques, methods, or strategies the practitioner and client are using to work toward the desired change.
So, in Janine’s case, the intervention section might read:
Therapist and client discussed gradual exposure techniques to start working up to completing a full in-person grocery shop.
Or a note from a session with an empowerment coach could state:
Discussed client’s limiting beliefs around her capacity to successfully launch an online business. Introduced the concept of focusing on strengths rather than weaknesses. Then, prompted the client to come up with some empowering affirmations she can use when self-doubt is becoming an issue. Assigned Quenza’s ‘You At Your Best’ Expansion to help the client identify her unique strengths.
Response
The response section provides an objective account of the individual’s reaction or progress in response to the intervention.
This is one of the most powerful parts of a GIRP note. It forces the practitioner to hone in on whether what they are doing in session is working and adjust course if necessary.
In coaching, an example would be:
Client struggled immensely with identifying strengths. By the end of the session we identified 3: creativity, persistence, and ability to learn new things. Did not get to move onto affirmations before the end of the session.
Plan
Where GIRP notes are similar to other formats, like SOAP and DAP, is that they always end with a plan.
The plan sets out the forthcoming steps, giving a clear roadmap for future treatment, services, and/or client tasks, based on insights gained from the individual’s response to past interventions.
For example, if Janine, who’s struggling with social anxiety got to her local supermarket and completed her grocery shop, the plan might be:
Janine to undertake 2 more trips for grocery shopping before next session. If successful, therapist and patient to decide on a new goal. May be suitable to include more social interaction, in line with long-term goal of having an active social life.
Benefits of GIRP Notes
The two most significant benefits of GIRP notes are that they enhance communication and maintain a focus on the individual’s goals.
Improved Communication
This clear, structured, time-bound, and goal-oriented nature of GIRP notes significantly enhances communication between the client and professionals involved in a case. The result is a collaborative approach to care and a strong therapeutic relationship, which is particularly important in a multidisciplinary and/or online setting.[1]
Focus On Individual Goals
By grounding each intervention in the desired outcome, the GIRP framework ensures that the chosen interventions and strategies remain directly relevant to the individual’s needs. This client-focused approach promotes ethical practice and can also enhance the effectiveness of therapy and coaching.[2]
How to Write High-Quality GIRP Notes
The process of writing an effective GIRP note involves a systematic and thoughtful approach.
Gather a Thorough History
To begin, the practitioner should gather a detailed collection of relevant information and observations about the individual, covering aspects such as:
- Demographic details
- Personal situation
- Social history
- Medical history
- Mental health background
- Personal preferences
- Presenting problem(s)
The information should be gathered through a combination of direct interactions with the individual, discussions with other professionals or family members, and a review of previous records. This ensures a comprehensive understanding of the individual’s needs and circumstances.
Set SMART Goals
Clients should always be in charge of identifying their own goals. But professionals may need to provide some support to translate goals into an actionable format.
While it’s not the only goal-setting framework, you can’t go wrong helping clients to set SMART goals.
To do this, simply guide clients through considering whether their goals are:
- Specific
- Measurable
- Attainable
- Relevant
- Time-bound
These goals should directly address the individual’s needs, offering a clear statement of what is to be achieved through the subsequent interventions. The process of goal-setting should primarily involve the individual, encouraging their participation and ownership of their care journey.
Use Person-Centered Interventions
Once the goals have been set, the professional then needs to develop intervention strategies.
These strategies should be derived from the professional’s expertise, knowledge of evidence-based practices, and understanding of the individual’s needs and preferences.
The chosen strategies need to be clearly aligned with goals, demonstrating a logical connection between what needs to be achieved and how it will be achieved.
Develop Action-Oriented Plans
After interventions are decided on, an action plan is created. This outlines the specific steps to implement the chosen strategies.
This plan should detail the:
- Timing, frequency, and sequence of the interventions
- Responsibilities of the client and different professionals involved
- Resources required
- Any necessary coordination with other services
- Anything else needed to enact or support the plan
The action plan essentially provides a roadmap for turning the chosen strategies into concrete actions.
Continually Evaluate Progress
After the plan has been put into action, its effectiveness is evaluated.
This evaluation should involve:
- Regular monitoring of the individual’s response to the interventions
- Recording any changes in their situation
- Progress achieved toward goals
- Any feedback or concerns raised by the individual
This ongoing evaluation provides crucial feedback on the efficacy of the interventions, informing necessary adjustments or changes in the plan.
Stay Objective
When writing GIRP notes, professionals should maintain a high degree of professionalism and objectivity.
Here are 3 tips for staying objective:
- Write in a clear, concise, and factual manner, providing an accurate account of the situation, without any personal opinions or biases.
- Respectful and non-stigmatizing language is encouraged, recognizing and maintaining the dignity of the individual.
- Professional assessments are ok, but any subjective interpretations or judgments should be avoided. The goal is to present a balanced and evidence-based account of the individual’s situation, interventions, and responses.[2]
Below we’ll provide more details, examples, and templates for GIRP notes, along with a discussion of how software programs like Quenza can assist.
Putting It All Together
To solidify what we’ve covered so far, here are some simplified GIRP note examples, tailored to various professional scenarios.
Let’s start with a scenario involving therapy for anxiety and panic attacks.
|
GIRP Heading |
Details |
|---|---|
| Goal | In this context, the goal could be reducing panic attack frequency |
| Intervention | May involve cognitive-behavioral therapy (CBT) techniques such as cognitive restructuring |
| Response | Might document the patient’s progress in understanding and applying these techniques, as well as any decrease in panic attack frequency |
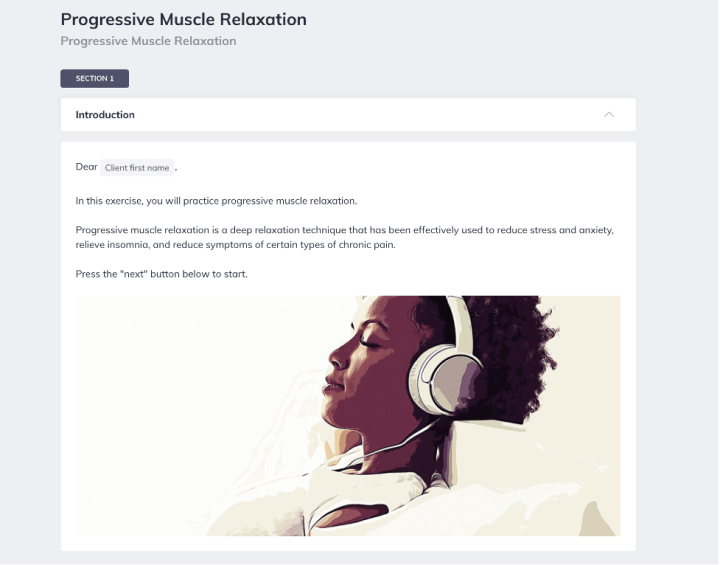
| Plan | Could involve continued CBT sessions and introducing relaxation techniques such as Quenza’s Progressive Muscle Relaxation |
And now an example from a performance evaluation context.
|
GIRP Heading |
Details |
|---|---|
| Goal | Might be improving an employee’s project management skills |
| Intervention | Could involve additional training or mentoring |
| Response | Would document the employee’s feedback on the training, any observed improvement in project management, and the impact on their overall performance |
| Plan | Might involve further advanced training sessions, practical assignments to apply the new skills, and regular feedback sessions |
Additional Tips
It’s crucial to analyze examples like this, not just for their content, but also for the underlying rationale.
Key points from both cases include:
- Goals were specific, directly related to the individual’s needs, and measurable
- Interventions were based on professional knowledge and aligned with the goals
- Responses were factual accounts of the individual’s reaction or progress
- Plans were clear roadmaps for future actions, directly derived from the observed responses
GIRP Notes Template
Using a premade template is one of the best ways to improve the efficiency and quality of your GIRP notes.
At a minimum, a template should have the GIRP headings. But many practitioners also find it useful to include short prompts for each section.
A good template means there’s no additional brain power needed to remember what should go under each heading. And as an added bonus, you’ve already got a mini-session plan written out to structure your appointment.
Example Template
|
Heading |
Prompts |
|---|---|
| Client Information | Basic details like name, date of interaction, and file/client number |
| Goal | A SMART goal for the client |
| Intervention | Detailed account of the specific intervention strategies used |
| Response | Objective documentation of the client’s response to the intervention |
| Plan | An outline of the next steps, including proposed interventions, meetings, or any necessary coordination with other professionals |
Each section of the template above serves a unique purpose, together forming a comprehensive and coherent narrative of the individual’s care journey. The template also ensures that each note maintains a consistent focus on the individual’s goals, the chosen interventions, the observed responses, and the subsequent plans.[1]
Where to Find a GIRP Notes Template
You can find GIRP notes templates online or make your own, using pen and paper or your preferred word processing program. Also, as we’ll discuss below, any good practice management software solution should include a customizable notes template.
Whatever you choose, the most important thing to remember is to adjust the template to suit your needs and experience level.
At first, you might include a detailed explainer and prompts under each heading. But as you become more familiar with the GIRP format, just the headings alone might suffice.
Furthermore, don’t forget to include any practice-specific requirements you might have in the template. This could include insurance details, diagnoses, or even basic reminders like the next appointment date.
Software for GIRP Notes
These days, most therapists and coaches use some form of note-taking and practice management software.
A good software solution has many benefits that can take the stress and hassle out of documentation, including:
- Auto-populating certain client details
- Secure messaging functionality
- Intuitively organizing and storing notes
- Pre-made, fully customizable templates
Each practitioner has different needs, so there’s no single right choice for everyone.
When comparing software for your needs, we suggest considering factors like ease of use (for practitioner and client), price, compatibility with existing systems, and additional features, such as scheduling or billing capabilities.
GIRP vs. BIRP vs. PIRP Notes
While GIRP notes focus on goals, BIRP notes (Behavior, Intervention, Response, Plan) center around behaviors.
On the other hand, PIRP notes (Problem, Intervention, Response, and Plan) prioritize problems over goals or behaviors.
Each documentation framework has its advantages and disadvantages, which may be more suitable for certain contexts. The right choice always depends on the specific situation, the individual’s needs, and the professional’s judgment.
Below is a quick-reference comparison guide for GIRP vs. BIRP vs. PIRP notes:
- GIRP notes emphasize the individual’s goals, promoting a more positive and proactive approach
- BIRP notes focus more on addressing problematic behaviors
- PIRP notes concentrate on solving problems
GIRP Notes in Quenza
Quenza is an intuitive software platform that allows therapists, coaches, and other healthcare professionals to increase client engagement, scale their practice, and provide automated care.
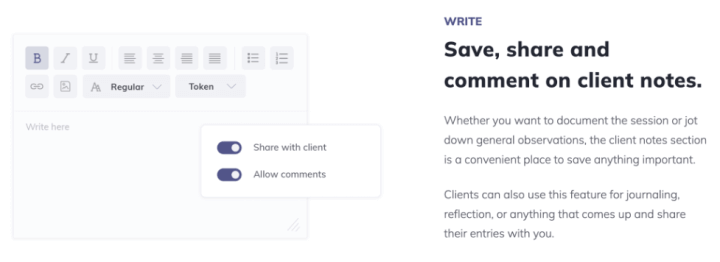
With Quenza Notes and our Activity Builder, you can use our full Expansions library to create HIPAA-compliant GIRP notes templates to your exact specifications. Alternatively, if one of our templates is already suited to your needs, you can simply use it as is.
All notes on Quenza can be written in real time during a session or any time afterward. And saving and sharing them with clients or other professionals is as easy as clicking a button.
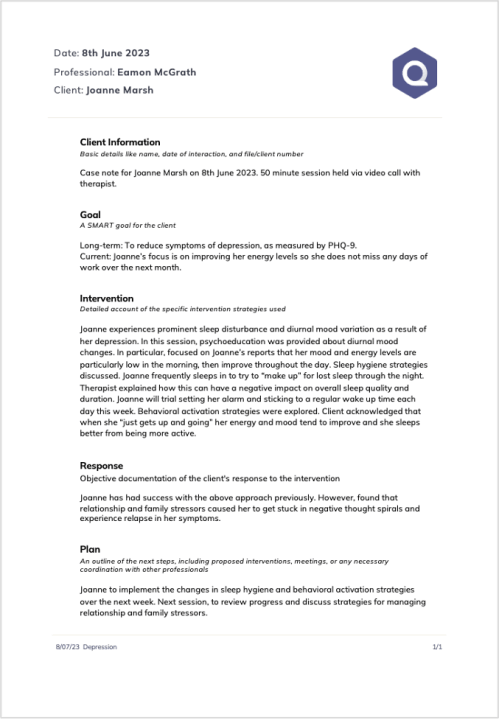
Example GIRP Note In Quenza
To show you what a GIRP note in Quenza might look like, we’ve provided a brief sample below, incorporating a treatment plan for depression.
Remember, you can customize templates to suit your needs and even print off a blank form to complete by hand if that’s your preference. To try it out for yourself, sign up for a 1-month free full-access trial today.
Common Mistakes to Avoid When Writing GIRP Notes
When writing GIRP notes, it’s essential to be aware of common pitfalls that can undermine the effectiveness of your documentation. One frequent mistake is being too vague in describing the goals and interventions. Goals should be specific, measurable, achievable, relevant, and time-bound (SMART), while interventions should clearly outline the therapist’s actions and techniques used.
Another common error is neglecting to update the notes regularly, leading to outdated information that does not accurately reflect the client’s current status. This can result in inadequate tracking of progress and missed opportunities for timely interventions. Additionally, some practitioners may overlook the importance of the client’s response, providing generic statements instead of specific observations and feedback. This component is crucial for understanding the effectiveness of the interventions and making necessary adjustments.
Finally, failing to plan appropriately for future sessions can leave both the therapist and the client without clear direction, hindering progress. By being mindful of these common mistakes, practitioners can ensure their GIRP notes are comprehensive, accurate, and useful for guiding therapeutic interventions.
Integrating Technology with GIRP Notes
Incorporating technology into the process of writing and managing GIRP notes can significantly enhance their efficiency and effectiveness. Various digital tools and software applications are available that streamline the documentation process, making it easier for therapists to maintain accurate and detailed records.
For instance, using electronic health records (EHR) systems allows for seamless integration of GIRP notes with other client information, providing a comprehensive view of the client’s history and progress. These systems often come with templates and prompts that ensure all necessary components of the GIRP framework are addressed, reducing the likelihood of omissions.
Additionally, digital tools can facilitate real-time updates, ensuring that notes are always current and reflective of the client’s status. This is particularly beneficial for tracking progress and making informed decisions about future interventions. Moreover, technology can enhance collaboration among multidisciplinary teams, allowing for shared access to GIRP notes and fostering a more coordinated approach to client care.
By leveraging the capabilities of modern technology, therapists can not only improve the quality of their GIRP notes but also save time and enhance overall client outcomes.
Final Thoughts
GIRP notes offer a systematic, goal-oriented approach to documenting individual care or coaching. They enhance communication among professionals and ensure client-centered care, by focusing interventions on the individual’s needs.
Writing effective GIRP notes requires a detailed understanding of the individual, setting SMART goals, developing aligned intervention strategies, creating a clear action plan, and conducting ongoing evaluation. Adherence to professionalism and objectivity is crucial in this process.
A high-quality template can greatly enhance efficiency when writing GIRP notes. Furthermore, many therapists and coaches find the template can double as a mini-session plan, ensuring the conversation stays on topic.
Quenza provides an all-in-one solution for writing progress notes, delivering therapy and coaching, running online programs, and much more.
To see how we integrate GIRP notes into our platform, and to try out the rest of our features, sign up for a 1-month full-access free trial today.
Frequently Asked Questions
GIRP notes offer a more structured and goal-oriented approach compared to traditional narrative progress notes. While narrative notes often provide a chronological account of a session, GIRP notes focus specifically on the client’s goals, the interventions used, the client’s response, and the plan moving forward. This structure ensures that each session is purposeful and aligned with the client’s objectives, making it easier to track progress and adjust treatment plans as needed.
Yes, GIRP notes can be adapted for use in group therapy settings. In this context, the “Goal” section might reflect a shared group goal or individual goals for each participant. The “Intervention” would describe the group activities or techniques used. The “Response” section could include observations about group dynamics and individual participant responses. Finally, the “Plan” would outline future group sessions and any individualized recommendations for participants.
To ensure HIPAA compliance when using GIRP notes, practitioners should:
- Use secure, encrypted software for electronic documentation,
- Include only relevant, factual information and avoid subjective judgments,
- Limit access to notes to authorized personnel only,
- Regularly update and review security measures,
- Obtain proper consent from clients for sharing information, and
- Ensure that any physical copies of notes are stored securely. It’s also crucial to stay updated on current HIPAA regulations and adjust practices accordingly.
In interdisciplinary care settings, GIRP notes can serve as a powerful communication tool. The structured format allows different professionals to quickly understand the client’s progress and treatment plan. To maximize effectiveness, each discipline can contribute to the notes, adding their specific interventions and observations. The “Plan” section can be used to coordinate care among team members, ensuring a cohesive approach. Regular team meetings to review and discuss GIRP notes can further enhance interdisciplinary collaboration and improve client outcomes.
To write concise yet comprehensive GIRP notes, practitioners can:
- Use clear, specific language and avoid jargon,
- Focus on key information relevant to each GIRP component,
- Use bullet points or short sentences to convey information efficiently,
- Incorporate standardized abbreviations where appropriate,
- Regularly review and refine note-taking skills, perhaps through peer review or professional development, and
- Utilize customizable templates that prompt for essential information while allowing for brevity.