Clear, concise, and accurate therapy progress notes are beneficial to practitioners and their clients. They’re instrumental in monitoring a patient’s progress, the efficacy of their treatment, and helping professionals understand their patient’s personal experiences.
To be helpful and informative, though, progress notes in mental health need to follow some guidelines. In this overview, we’ll introduce their key elements, a step-by-step guide to writing therapy progress notes, and some of the best therapy software you can use to create excellent progress notes efficiently.
Before getting started, we recommend trying Quenza, our therapy notes software for e-mental health practitioners.
Quenza is a complete suite of blended care tools that includes everything you need to make and store clear, professional therapy progress notes on a HIPAA-compliant platform.
What Are Progress Notes in Mental Health?
Progress notes are clinical notes made by psychologists, therapists, clinical counselors, psychiatrists, and other practitioners involved in a patient’s treatment and care.
More specifically, they contain clinical facts and medical reasoning about “the care delivered to patients and the clinical events relevant to diagnosis and treatment.”[1]
Progress notes are professional documents that communicate important information on a patient’s condition between multiple providers. In mental health contexts, they must be stored privately and securely in a HIPAA-compliant manner.
Difference Between Progress & Psychotherapy Notes
Progress notes are professional documents that communicate important information on a patient’s condition between multiple providers.
As medical and mental healthcare providers will know, progress notes play a vital role in treatment planning and service delivery across a wide range of helping professions, such as occupational, physical, and speech therapy.
This distinguishes them from psychotherapy notes, which contain information exclusively related to a patient’s therapy sessions. Also, unlike progress notes, psychotherapy notes are only written by counselors, therapists, and mental health practitioners who are actively involved in their therapy.
This table outlines a few more differences between progress and psychotherapy notes.
|
Progress Notes |
Psychotherapy Notes | |
|---|---|---|
|
Purpose |
|
|
|
Written by |
Any care provider involved in a patient’s treatment plan, e.g., Social/Case Workers, GPs. |
Psychologist, Psychiatrist, Counselor, Psychotherapist |
|
Content | May include:
| May include:
|
|
Privacy |
|
|
10 Steps For Writing Effective Progress Notes
Following a template is an easy way to ensure all important details and information are included in your therapy progress notes.
Many treatment software solutions offer this functionality, with a variety of formats and outlines for different healthcare subsectors – psychiatry, counseling, and more.
For instance, Therapy Notes comes with Psychotherapy Progress Notes templates and a step-by-step guide to help psychologists write effective progress notes. Each step corresponds with a different field in the note, starting with patient information and ending with a digital clinician signature:[2]
- Note Header: A brief overview of the essential practitioner, patient, and session information, such as when the appointment took place, its duration, and service codes for practice administration.
- Diagnosis: ICD-10 or DMS5 codes might be relevant here if the patient has been diagnosed with a mental health condition.
- Patient Presentation: A description of how the client appears, using different modalities, e.g., cognitive functioning, affect, or behavior.
- Safety Issues: Any important information regarding the patient’s well-being.
- Medications: For prescribing clinicians such as psychiatrists and general MDs.
- Symptom Description and Subjective Report: This includes reports and direct quotes regarding the patient’s status. These may come from the client themself and/or their key caregiver and might relate to how the patient is feeling, how they view their progress, or their opinions on the mental health treatment plan.
- Relevant Content: Objective data such as test results, documents, and therapy notes might be included here – this section is for relevant e-mental health information that could ‘complete the picture’ drawn by the progress note.
- Interventions Used: This step involves documenting the treatment interventions applied and the broader field that they fall into. Examples might include cognitive restructuring within CBT or relaxation techniques as part of a mindfulness training program.
- Treatment Plan Progress: Each progress note should mention whether a client’s treatment plan objectives are being met.
- Signatures: Most telecounseling software includes the ability to e-sign documents and store them in a secure, HIPAA-compliant manner.
A Brief Look At The SOAP Method
If the step-by-step guide above seems familiar, it’s likely because this particular therapy progress notes template leverages central elements of the SOAP note format.
SOAP Notes follow a standard 4-point layout covering critical information on a patient’s health status. A specific type of progress note, SOAP notes can be shared with any other therapists and care professionals the client may be working with.
The four sections of a SOAP method note are:
- Subjective Data on a patient’s feelings, experiences, or thoughts, such as direct quotes or their observations
- Objective Data regarding their mental or general health status, e.g., details from their therapy appointment
- Assessment Information that integrates subjective and objective details with a therapist’s professional interpretation, and
- Plan details regarding any adjustments or next steps that the counselor and client feel are needed.
Read Writing SOAP Notes: Step-by-Step Guide, Examples, and Templates for a little more detail on what each section should feature, as well as a host of helpful formats and walkthroughs. If you are an occupational therapist, read How to Write Occupational Therapy Soap Notes for more information and some examples.
3 Helpful Templates and Formats
Therapy progress notes can range from the very basic to more comprehensive, detailed structures.
SOAP Notes aren’t the only format used in mental health documentation. Mental health progress notes can range from the very basic to more comprehensive structures, like the 10-step example Therapy Notes above.
To illustrate, here are some useful free templates for practitioners to use and download.
Quenza Therapy Notes Templates
Quenza offers free evaluation, assessment, and intake document templates for e-counselors in its Expansion Library, including a range of forms that can be customized to use as therapy progress note templates. For example, the End of Therapy Evaluation captures data on a client’s overall feedback on their progress for inclusion in progress notes.
These insights can help practitioners keep track of how a client is progressing with therapy and can be used to populate more detailed therapy notes that include the session’s focus, client’s name, and more. With professional therapy notes software, this is often as simple as including custom fields for additional information.
SampleTemplates
SampleTemplates also provides healthcare progress notes formats for physical therapists, pediatricians, general clinicians, and therapists.
These include BIRP Note templates, SOAP Note structures, integrated progress notes and billing forms, and digital samples for electronic note-taking.
HarmResearch.org
HarmResearch.org sells Psychiatric and versatile Visit Progress Note templates for professional use. Their psychiatric progress note template includes fields for:
- Patient demographics
- Presenting problem
- Past psychiatric history
- Diagnostic interview summaries
- Past medical history, and other key fields.
List of Interventions & Common Terminology
When documenting interventions and treatments as part of progress note-taking, appropriate language and abbreviations can greatly speed up the process.
Clinical terminology also ensures a common professional language exists between practitioners; it facilitates better understanding and establishes a consistent frame of reference.
In therapy for mental health, appropriate terminology can be a combination of diagnostic references, such as DSM5 or ICD-10 codes, and descriptive terms for subjective sections progress notes.
Common Terminology
The County of Santa Clara suggests a helpful Counselor’s Thesaurus in its Clinician’s Guide Toolkit. This covers commonly-used descriptors to detail different aspects of a client’s health, appearance, and more.[3]
The Thesaurus covers categories such as:
- Affect, Mood, or Disposition – e.g. Lighthearted/carefree, Depressed/Dejected/Dispirited/Disheartened, Flat/Shallow/Dull/Listless
- Attitude – such as Apathetic/Inert/Absence of Affect, Belligerent/Quarrelsome/Disagreeable
- Behavior – ideas include Over-cautious/Too Careful, Lethargic/Sluggish, or Spontaneous/Immediate
- Work Habits, Cognition, Orientation, and more.
Interventions
Having a list of frequently-used interventions on hand for quick reference can be particularly useful in multi-provider contexts, helping different practitioners understand what treatments a client is pursuing with other specialists.
In mental health disciplines, these interventions might address:[4]
- Anger Management for healthier self-expression
- Behavior Reinforcement, commonly part of intrinsic coaching methodologies
- Collaborative Problem-solving for relationship counseling, family therapy, conflict resolution, and other
- Cognitive Restructuring – a thought-based CBT intervention
- Communication Skills Development – e.g., as part of interpersonal therapy
- Coping Strategies Development for addressing a diversity of mental health conditions
- Eye Movement Desensitization and Reprocessing (EMDR) for trauma counseling
- Progress/Objective Review, which might involve collaborative goal-setting as part of mental health coaching
- Identifying Triggers, as seen in therapy for substance abuse, or anger management
- Imagery – e.g., within a graded exposure treatment for anxiety
- Mindfulness – covering Mindfulness-Based Stress Reduction (MBSR), Mindfulness-Based Cognitive Therapy (MBCT), and formal/informal Mindfulness Training
- Problem-Solving Skills Development – another versatile CBT intervention, and
- Stress Management – which can include both therapist-guided activities and lower-intensity Stepped Care interventions.
Individual & Group Therapy Notes: 3 Examples
Progress notes for individual and group therapy will differ in a few ways, as different sections may be required for distinct criteria. Their overall purpose, however, remains the same.
This means that both documentation types should include details on the particular patient or client’s progress overall, important identifiers, and relevant notes from the session that took place.
The snapshot below shows part of an Individual Progress Note created using the ICANotes software, in which behavior, content of therapy, intervention, diagnoses, and treatment plan details are included:[5]

Comparing this with an ICANotes Group Therapy Progress Note Example, we can see the latter varies only slightly with regard to structure and content.

Both individual and group therapy notes are legal documents and must be stored securely.
Another clever way to integrate subjective data into therapy progress notes is by inviting clients to contribute their own notes from sessions.
One example template in Quenza’s Expansion Library, Session Notes for Clients, offers a structured form for patients to fill out with insights, reflections, and other observations from a therapy appointment:
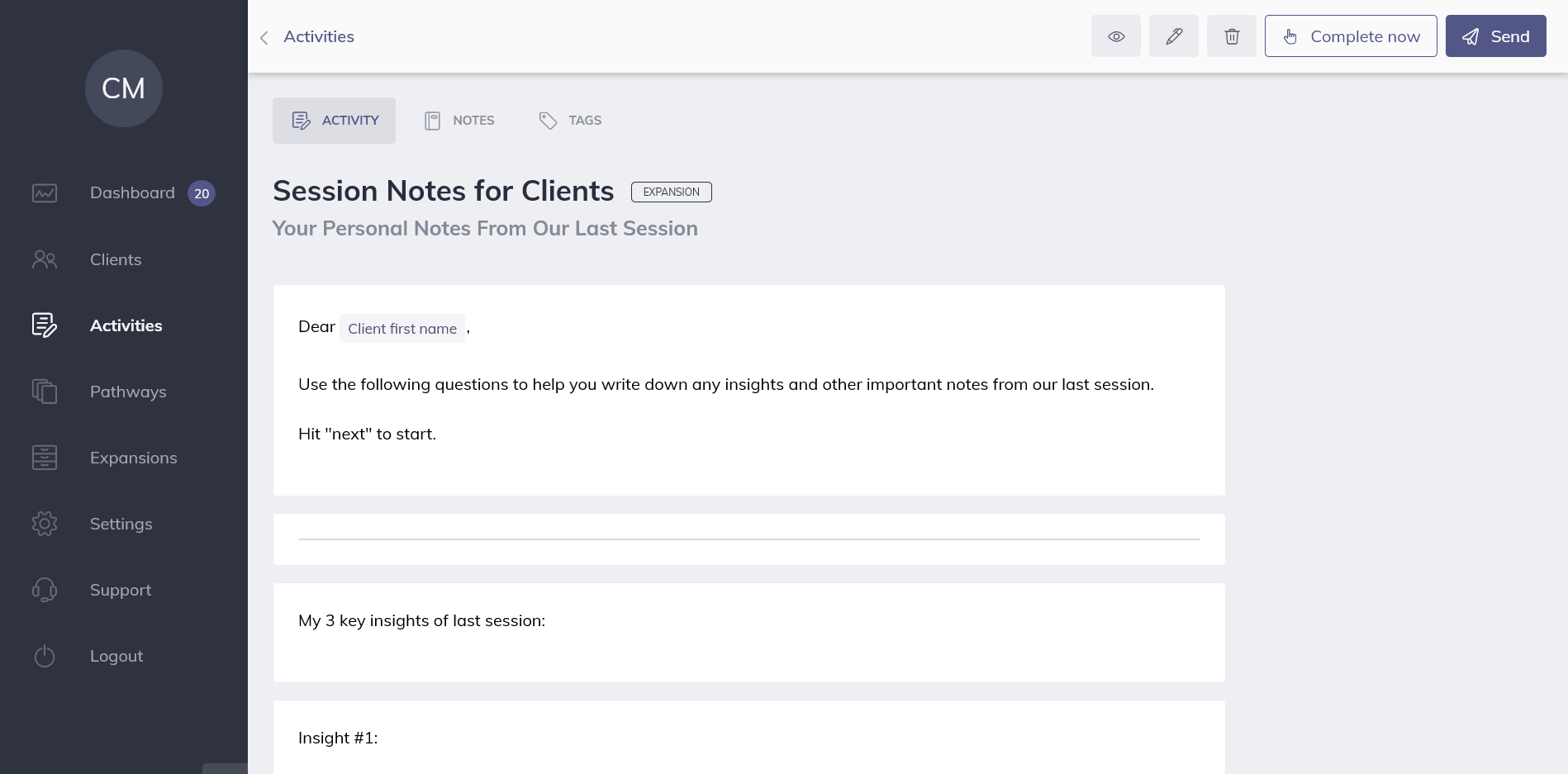
By collecting a patient’s own observations online, professionals can easily copy and paste direct quotes into their private progress notes. All data is securely stored on the one HIPAA-compliant therapy platform, and visible only to the client and their therapist.
Smart Solutions: 3 Apps and Software Systems
Whether you’re looking for a lightweight, dedicated Progress Notes software or a bigger solution, these apps and systems all come with templates for therapists and other mental health specialists.
|
Software |
Details |
|---|---|
 | MyClientsPlus is a versatile mental health system for small practices and solo practitioners – it’s also relatively simple to use after an initial learning curve. With MCP’s Therapy Progress Notes capabilities, counselors and psychologists can choose between templates for psychiatry, counseling, general psychology, and more.Within different sub-sectors, you’ll find even more predesigned formats to make documentation more effective and efficient. Examples include Therapy Intake Forms, Treatment Plans, and Client Information Forms.MyClientsPlus further streamlines Progress Note creation with diagnostic codes and e-signatures and is one of the more affordable solutions on the market. |
| Name | MyClientsPlus |
| Price | $24.95+ monthly |
| Good For | Psychologists, e-Counselors, Therapists, Mental Health Coaches |
| Website | https://www.myclientsplus.com/ |
|
Software |
Details |
|---|---|
 | Both mental health treatment plans and progress notes are easy to create with Quenza’s browser-based software and apps.Templates for different note types, such as SOAP notes, BIRP notes, and more can be built quickly using drag-and-drop tools, and the software stores all progress notes privately and securely on a GDPR- and HIPAA-compliant system.Forms can be shared through a private Portal on free client iPhone and Android apps, and all progress and results are shared in real-time with the therapist. Even better, Quenza comes with a huge Expansion Library of freely customizable note templates. |
| Name | Quenza |
| Price | $25+ monthly |
| Good For | Psychologists, e-Counselors, Physical Therapy, Speech Therapy, Occupational Therapy, Mental Health Coaches, Mental Health Apps |
| Website | https://quenza.com/ |
|
Software |
Details |
|---|---|
 | TherapyNotes has a library of Progress Note templates for solo practitioners and teams and comes with video therapy software for telehealth sessions.Psychotherapy Progress Notes, as shown above, can be populated using clinical codes before they are linked with a client’s appointments for easier admin and use in sessions. When a Therapy Session starts, the software automatically creates a To-Do list item reminding users to create the relevant documentation. |
| Name | TherapyNotes |
| Price | $49+ monthly |
| Good For | Psychologists, e-Counselors, Therapists, Mental Health Coaches |
| Website | https://www.therapynotes.com/ |
Enhancing Client Engagement Through Progress Notes
Engaging clients effectively is crucial for successful therapeutic outcomes. Progress notes are not just for documentation; they can also play a role in fostering client engagement. When clients are aware that their progress is being meticulously tracked, it can motivate them to stay committed to their therapeutic goals.
One way to enhance engagement is by sharing parts of the progress notes with clients. This transparency helps clients understand their journey and see the tangible progress they are making. It can also facilitate more open communication between the therapist and the client, making the therapeutic process more collaborative.
Another strategy is to involve clients in the note-taking process. For instance, at the end of a session, a therapist might ask the client what key points they would like to be noted. This involvement can empower clients, making them feel more invested in their therapy. It also ensures that the notes accurately reflect the client’s perspective.
Using progress notes as a tool for setting and reviewing goals can be highly effective. By regularly referring to the notes during sessions to track progress against the goals, clients can see their achievements and areas needing more focus. This ongoing review process can boost motivation and reinforce a sense of accomplishment.
Leveraging Technology for Effective Progress Notes
The advent of digital tools has revolutionized the way therapists manage progress notes. Utilizing specialized software can streamline the documentation process, ensuring that notes are thorough, organized, and easily accessible.
Digital tools offer several advantages. Firstly, they can integrate with other practice management systems, allowing for seamless updates and retrieval of client information. This integration ensures that all relevant data is centralized, making it easier for therapists to access and review past notes.
Moreover, many digital platforms offer templates and prompts that guide therapists in what to include in their notes. This can be particularly helpful for ensuring that all critical aspects of the session are documented, from client behavior to treatment responses. These features help in maintaining consistency and comprehensiveness in note-taking.
Another benefit is the ability to securely store and share notes. With proper encryption and security measures, digital notes can be shared with other healthcare providers involved in the client’s care, facilitating better coordinated care. Additionally, secure sharing options can also make it easier to involve clients in the review process, enhancing transparency and engagement.
Leveraging technology not only makes the documentation process more efficient but also enhances the quality of care provided. Digital tools ensure that progress notes are detailed, easily accessible, and securely stored, contributing to better therapeutic outcomes.
Final Thoughts
From basic SOAP frameworks to detailed psychiatry notes, there’s no one way to write a great progress note. The way you choose to document your client’s information is down to you as a practitioner, but hopefully, these templates, guides, and formats will be of value.
If you’re happy with your Therapy Progress Notes software, do let your fellow professionals know in a comment. If you’re still on the hunt for a new solution, you’ll find even more tips and advice in our comprehensive article on therapy notes software.
We hope you’ve found some clever ways to streamline your therapy documentation. To implement what you’ve learned, don’t forget to explore Quenza’s Therapy software tools with your free 30-day trial.
If your goal is to have a bigger positive impact on your clients’ wellbeing, Quenza will give you everything you need to create professional, accurate notes more efficiently, leaving you with more time to focus on the mental healthcare solutions that matter.
Frequently Asked Questions
Therapy progress notes should generally be concise yet comprehensive, typically ranging from 1-2 paragraphs to a full page. The length may vary depending on the complexity of the session, the client’s needs, and any significant developments. The key is to include all relevant information without unnecessary details, focusing on the client’s progress, interventions used, and plans for future sessions.
To maintain client confidentiality in progress notes, therapists should: use client initials or codes instead of full names, store notes securely (preferably in HIPAA-compliant digital systems), avoid including unnecessary personal details, focus on clinical observations rather than personal judgments, and limit access to notes to only those directly involved in the client’s care. It’s also important to inform clients about how their information will be used and stored.
Common mistakes to avoid include: being too vague or overly detailed, using subjective language instead of objective observations, failing to document important clinical decisions or risk assessments, neglecting to update treatment plans, and not noting the client’s progress towards goals. It’s also crucial to avoid including personal opinions or non-clinical information that doesn’t directly relate to the client’s treatment.
Therapists should review and update their progress note templates at least annually, or more frequently if there are changes in professional standards, legal requirements, or organizational policies. Regular reviews ensure that templates remain current, efficient, and aligned with best practices. It’s also beneficial to adjust templates based on feedback from supervisors or peers, and to accommodate any changes in therapeutic approaches or client populations.
Therapists can use progress notes as a tool for self-reflection and improvement by: regularly reviewing past notes to identify patterns in client progress or their own interventions, using notes to prepare for supervision sessions, analyzing the effectiveness of different therapeutic techniques across clients, and setting personal development goals based on trends observed in their documentation. Additionally, thorough progress notes can help therapists track long-term client outcomes and adjust treatment strategies accordingly.
References
- ^ Aghili, H., Mushlin, R. A., Williams, R. M., & Rose, J. S. (1997). Progress notes model. In Proceedings of the AMIA Annual Fall Symposium (p. 12). American Medical Informatics Association.
- ^ Therapy Notes. (2020). How To: Complete a Progress Note. Retrieved from https://support.therapynotes.com/article/118-how-to-complete-a-progress-note
- ^ Santa Clara County. (2008). Clinician's Guide Toolkit. Retrieved from https://www.sccgov.org/sites/bhd-p/Policies-Procedures/adult-system-of-care--policy-procedure/Documents/Clinician_Gde_toolkit.pdf
- ^ MyClientsPlus. (2020). Commonly-used Intervention Words for Mental Health Progress Notes. Retrieved from https://myclientsplus.com/blog/commonly-used-intervention-words-for-mental-health-progress-notes/
- ^ ICANotes. (2020). Sample Notes Therapy Notes. Retrieved from https://www.icanotes.com/features/charting/therapy/sample-notes/


are these soft wares only applied for online counseling or they can be applied my offline therapies.
how is confidentiality guaranteed?
Hi Jimm,
The software can be used by all types of helping professionals, whether it be coaches, counselors, or therapists.
Learn more about how confidentiality and security is guaranteed at: https://support.quenza.com/knowledge-base/privacy-data-security/
Thank you!
I will like to use it to improve my progress note writing for billings in the near future. I’m an addiction counselor working for a non-profit organization and will like to have a more structured temple for my progress notes.
That’s awesome Sandra, we’re so happy to hear it 🙂
You might also find the Quenza Notes feature very useful too: https://quenza.com/blog/quenza-notes-journaling/
Best of luck with your work!