Contents
You don’t have to use therapy notes software. But for any practitioner who’s switched from manual to digital note-taking—it’s impossible to imagine going back.
Most therapists find that note-taking softwares considerably improves the efficiency and quality of care they deliver. Whether it’s the ability to write and access notes from anywhere, convenience of ready-to-use intake and assessment forms or time-saving customizable templates and integrated billing functions.
However, for utilizing all of its benefits, choosing the right product for your needs isn’t an easy task.
You’ve got to consider cost, features, and integration with your existing digital tools. And that’s even before you think about things like compliance with security and privacy laws.
To help you make the right decision, we’ll break down everything you need to know about therapy notes software in this article.
We’ve included a section comparing the top products. And as we go along, we’ll detail practical examples from Quenza, so you can see exactly how digital therapy tools can enhance your practice.
If you want to try out Quenza today, you can get full access right now by signing up for a free full-access 1-month trial.
Chapter 1
The Secrets to Effective Notes
High-quality documentation in therapy is a non-negotiable for meeting professional and legal standards. It’s also required by insurers and funding bodies, who may periodically request an audit for costs they have incurred for your services.
However, therapy notes aren’t just about ticking boxes or maintaining a record.
When used thoughtfully, documentation can be a powerful way for you to enhance the standard of your practice and improve client outcomes.
Below are some of the benefits of using software for therapy notes.
Holistic Overview of Patient’s Journey
By having organized documentation and progress notes, therapists can better track a patient’s progression, pinpointing areas of improvement and those that need more focus. This clear chronicle of each session and assessment aids in building a more structured and informed plan, which can result in improved clinical outcomes[1].
Because therapy note software stores all documents in one place (such as intake forms, assessments, and session notes), it’s a breeze to conduct an overall review with or without the patient. You can also securely share notes and information, without having to worry about printing or photocopying pieces of paper.
Protects Patient Confidentiality
With rising concerns about confidentiality and security, therapists must ensure their patients’ sensitive information remains protected from unauthorized access.
Contrary to popular belief, paper notes are less secure than electronic notes.
Traditional paper notes can be lost, stolen, damaged, copied, or viewed by unauthorized parties. But electronic notes, when managed properly, offer layers of security encryption[2]. Furthermore, unlike paper notes, electronic records can automatically keep an accurate timestamp of who has accessed them.

Streamlines the Administrative Process
While the presence of a well-maintained digital record can make therapy more effective, that doesn’t mean the time spent on documentation always results in a net positive for the patient and clinician.
Spending too much time on notes can take away from valuable clinical time. This not only limits your ability to deliver care. It also reduces your income, productivity, or both.
Intelligent therapy progress notes software makes every aspect of documentation and record keeping more efficient. Plus, it can include various time-saving features to reduce administrative load, such as automated reminders, templates, and an integrated medical billing system.

Chapter 2
Key Features
With the huge number of options available, finding the perfect software can be daunting.
One way to narrow down the list to just the best products is to check for 4 key features that are common to all best therapy notes software products.
- User-Friendly Interface. Therapy is intricate, but your software shouldn’t be. A clean, intuitive interface ensures that therapists can focus on their notes rather than navigating a complicated system. Easy note-taking, coupled with quick retrieval mechanisms, makes for efficient sessions.
- Security Measures: Look for software that prides itself on its security features. HIPAA compliance is non-negotiable. Encryption tools, multi-factor authentication, and regular security audits further elevate a software’s integrity.
- Customizability: Every therapist has their unique style, and so should their software. Whether tailoring notes for individual sessions or adapting them for various therapeutic methods like CBT or group therapy, the software should be flexible.
- Integration Capabilities: In a clinic (or even a busy solo operation), various systems need to work in harmony. Appointment scheduling, billing, and patient communications are some examples. Therapy notes software that integrates seamlessly with other tools used in your practice can be a game-changer.
Chapter 3
Comparing Therapy Notes Software
The right software can significantly enhance the experience for both therapists and their patients. The challenge is, the type of therapy you’re delivering might require specific software features.
Let’s delve into the different types of therapy notes software to explore this further:
Psychotherapy Notes Software
Tailored for psychotherapists, electronic psychotherapy notes software is designed with in-depth analytical features.
Psychotherapists often require tools that allow them to chart intricate details of patients’ emotional and cognitive responses.
Features such as customizable templates for different psychotherapeutic techniques, integrated scales, and mood trackers can make the note-taking process more comprehensive.
The Expansions library in Quenza has dozens of CBT-based psychotherapy tools, like the one below on Unhelpful Thinking Styles – Magnification and Minimization.
Software for Group Therapy Notes
Managing group therapy sessions comes with its own set of challenges, mainly around handling multiple patients (and their records) simultaneously[3].
Group therapy notes software usually offers features that allow therapists to tag individual participants, note group dynamics, track individual progress within the group setting, and maintain a record of group activities and interactions.
Quenza Groups includes all the tools you need to run group therapy sessions in person or online.
Psychology Therapy Notes Software
Designed for psychologists, this software often integrates tools for standardized testing and assessments.
Psychology notes software is designed to assist in recording observations, test results, and behavioral patterns.
Integration with popular psychological assessment tools and databases can provide added value as well.
Counseling Notes Software
Counselors need a system that’s adept at handling goal-oriented therapy, abstract emotional concepts, and relevant therapeutic approaches.
Such software often comes with goal-setting tools, progress trackers, and templates designed for short-term interventions.
Counseling notes software should also give the option for easy communication between sessions, allowing for expanded support.

Quenza includes a range of features for therapists, counselors, and psychologists. Get full access now by signing up for a free full-access 1-month trial.
Common Features for All Therapy Notes Software
Beyond the specifics of therapeutic methodology, look for these 3 features in any electronic psychotherapy notes product you’re considering purchasing.
- Cloud Integration. Digital notes can be backed up to the cloud, ensuring they’re safe from physical harm or loss.
- Security Features. Security features like encryption ensure that patient data remains confidential.
- Accessibility. Therapists can access their notes from anywhere, facilitating remote sessions or consultations while on the move.
Chapter 4
From Manual to Digital Therapy Notes
As the world has gravitated towards digital health solutions, the field of therapy followed suit[4].
While by no means comprehensive, the points below sum up several of the key steps in the transition from manual to electronic therapy notes.
Evolution of Therapy Note-taking
Traditional note-taking, often confined to paper and pen, had its charm.
The tactile nature of writing could sometimes assist in the processing of therapeutic content. However, with the advent of digital tools, most therapists found they could achieve greater efficiency, organization, accuracy, and security with electronic documentation.
Fortunately, these days writing in-session notes electronically doesn’t require sitting behind a PC with a large screen. A compact notebook computer or tablet that’s no more obtrusive than a pad and pen can be used.
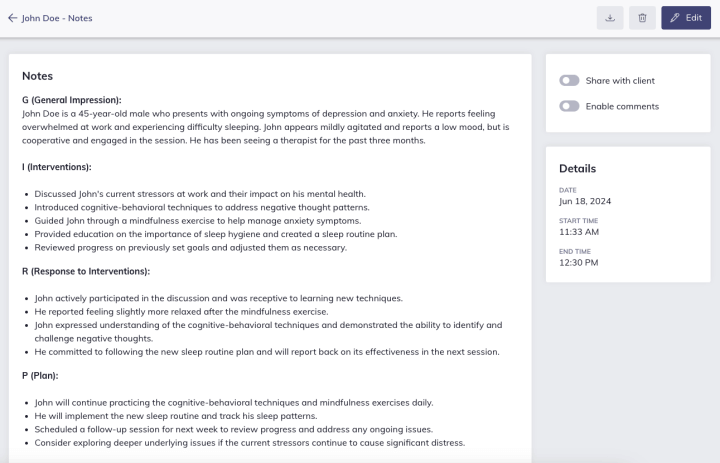
Example of a GIRP note written using Quenza’s pre-made template.
Benefits of Electronic Therapy Progress Notes
Digital note-taking has several advantages over paper-based records.
- Instant searchability ensures that therapists can quickly reference past sessions
- Integration capabilities mean billing, scheduling, and notes can be in one unified system
- Electronic notes can be easily shared, aiding in coordinated care or supervision
These benefits all facilitated the rapid and widespread adoption of therapy note software among clinicians. And, they mean few would ever consider going back to a paper-based alternative.
Chapter 5
The Pros & Cons of Therapy Note Software
Like any tool, therapy note software offers a mix of advantages and potential pitfalls. It’s essential to weigh these before making an investment.
Pros:
- Improved Organization: With digital software, sifting through piles of paper becomes a thing of the past. Therapists can easily categorize, tag, and search through their notes.
- Security: High-quality software ensures that data is encrypted and stored securely, adhering to HIPAA guidelines.
- Efficiency: Automated templates, reminders, and integration features can significantly reduce administrative time.
- Accessibility: Digital notes can be accessed from various devices, making remote sessions and consultations seamless.
Cons:
- Learning Curve: It might take time for therapists to adapt to new software, especially those accustomed to paper-based methods.
- Potential Tech Issues: Like all software, there’s always a chance of running into bugs or technical glitches. These can be frustrating and kill productivity.
- Costs: Some of the best software can come with a hefty price tag, especially for premium features.
Chapter 6
Top 5 Therapy Notes Software 2023
If you want a head start in your search for the best therapy notes software for your practice, check out our top 5 picks for 2023.
The products below vary from specific note-taking apps to full-feature electronic health records (EHRs) and practice management systems. And to help you make the right choice, we’ve even included details on pricing, pros, cons, and examples of user feedback.
| App | Details |
|---|---|
 | Some electronic psychotherapy notes products try to cram in as many features as possible, inflating the price without adding value to the user—but not Note Designer. Note Designer is a simple, effective, no-frills therapy notes software product that does exactly what it promises: Helps you write better notes, faster. If you’re looking for an affordable product that just helps you with writing notes, this is one of the best choices on the market today. |
| Pricing | Group and individual plans start from $12 per month, with discounts if you take out an annual plan. |
| Pros | Huge library of notes templates (e.g., SOAP, BIRP, DAP)Over 400 set phrases and statements allowing “pre-filled” notes to review and adjust as neededSimple, easy-to-navigate user interface |
| Cons | Expanded features beyond note-taking are limitedAffordable as a standalone product, but perhaps not if you also need an EHR or other therapy softwareNo app (only runs in web browser) |
| User Feedback | “This software has already saved me hours of work and a truckload of frustration. Thanks!”R.R., MAFT |
| App | Details |
|---|---|
| While mainly branded as counseling notes software, CounSol is a solid choice for any mental health professional. As a full practice management system and all-in-one EHR, CounSol combines robust digital note-taking features with everything else you need to run a thriving therapy business. CounSol even has a secure and encrypted video chat feature, so you can work from anywhere in the US with a reliable internet connection | |
| Pricing | Basic plan – $34.95 per month; Premium plan – $59.95 per month |
| Pros | Customized notes templates and ready-made formsOnline booking and appointment remindersComprehensive insurance and billing features |
| Cons | Expensive if you don’t need all the featuresNo free plan (although a 14-day free trial is available)Limited integration with other software products |
| User Feedback | “CounSol has helped a great deal with building my counseling business. I have been using them for 6 years and the service has been most amazing in reducing no shows and managing billing. My clients are also happy with the ease of reviewing and signing forms online and receiving appointment reminders. Perfect for counselors!”L.G., LPC |
| App | Details |
|---|---|
 | Designed with the specific needs of therapists, counselors, and coaches in mind, Quenza is a unique product in the software world. This is because Quenza doesn’t just handle the administrative tasks of running a therapy business—it also helps substantially on the clinical side. Quenza takes care of all aspects of documentation, with customizable notes templates, assessment forms, and even client-practitioner contracts. You can use all of these as-is or adjust them to suit your specific needs. And everything is stored in a HIPAA-compliant cloud-based platform that can be accessed via the web or our mobile apps. In addition to administration and note-taking features, Quenza includes a full suite of digital clinical tools with all levels of subscription. You’ll need to check out the website for the full list of features, but some stand-outs are: An extensive library of 250+ science-based digital therapy toolsFunctionality to run groups, build online courses, and collaborate with other professionals (all standard inclusions)A secure client portal with advanced communication featuresImport your own resources or customize ours to be your own with white-label functions |
| Pricing | From $25 per month |
| Pros | Administrative and clinical tools included in one productAdvanced tools to deliver automated care and engage clients between sessionsAllows you to grow your business by diversifying service offerings (e.g., online courses and group therapy/coaching) |
| Cons | Not every practitioner will use such a broad range of featuresInsurance and billing features are limitedMore expensive than a notes-only software product |
| User Feedback | “Quenza saves me time by making my communication with my clients easier. All my client documents are in one place so I’m not hunting around because I’ve lost track of which email had which document. My clients also enjoy using it. Quenza is an aesthetically beautiful platform so I enjoy being on it. It allows customization so my business appears more professional.”U.A., Therapist and Practice Owner |
| App | Details |
|---|---|
| An all-in-one EHR for healthcare practitioners of any kind, CarePatron helps therapists create high-quality documentation with minimal fuss. CarePatron includes a comprehensive suite of clinical note-taking and documentation features. And allows you to store all client-related and administrative material safely in a secure EHR system. With per-user pricing, CarePatron can be an affordable option for solo or small group practices. | |
| Pricing | $0 – $19 per staff user |
| Pros | Great selection of customizable note templatesIntegrates with other practice management software toolsOne of the few therapy notes software products to offer a free version |
| Cons | Not all features available on the mobile appNo built-in telehealth featureFree plan has limited features and customizability options |
| User Feedback | “Excellent experience. I was searching for an EHR suitable for a solo practitioner in the mental health space. I did a ton of research and test-drove at least 15 EHRs. Carepatron was the obvious choice based on personalized onboarding and customer support, features, and ease of use.”A.A., RMHN |
| App | Details |
|---|---|
 | Built by therapists, for therapists, TheraNest was one of the first behavioral health-specific software for therapy notes products to come on the market. With the needs of mental health and substance misuse professionals in mind, TheraNest includes all the note-taking and practice management features you’d expect from any good EHR. But it also comes with comprehensive billing and revenue cycle management (RCM) capabilities as well. |
| Pricing | $39 – $49 per user a month |
| Pros | A comprehensive EHR that can handle all administrative and clinical needsIntegrated DSM-5 ready notes and assessment toolsThe option of several advanced add-ons to expand functionality |
| Cons | One of the more expensive products on the marketSomewhat complex user interfaceNot all clinicians will need the billing and RCM tools |
| User Feedback | “TheraNest is full featured- Our office used a competitor program for 30+ years but wanted/needed a cloud based state of the art EHR program- Our office tried several other popular programs but they all had significant limitations. We are very excited about Theranest.”G.S., Clinical Psychologist |
Final Thoughts
In the evolving landscape of mental healthcare, having reliable therapy notes software is no longer a luxury—it’s a necessity.
As therapists, our primary goal is to provide the highest standard of care possible. And the right tools can significantly assist in this area.
The best therapy notes software products don’t just save you time on administration. They also include a range of clinical tools and communication features that enable you to go deeper with clients during and between sessions, making the overall process of therapy more effective.
Before committing to a product, it’s crucial to conduct thorough research, consider individual practice needs, and possibly even trial a few options.
We’ve covered everything you need to make the right choice in this article. And if you want to try Quenza out today, remember you can sign up now for a free full-access 1-month trial.
Frequently Asked Questions
Counseling software typically focuses on goal-oriented therapy and shorter-term interventions, while psychotherapy software dives deeper, accommodating intricate emotional and cognitive response tracking.
Choose HIPAA-compliant software, always enable multi-factor authentication, and ensure regular backups. It’s also wise to stay updated with software patches that address security vulnerabilities.
Yes, several software options offer basic features for free, but advanced features might come at a cost. Always read user reviews and ensure any free software still meets security standards.
Regular backups are crucial. Daily backups are ideal. But at a minimum, consider weekly backups. Many cloud-based options offer automatic backups.
Most quality therapy notes software allows template customization to suit individual therapeutic methods and client needs. Before committing, trial the software to ensure its customization meets your standards.
References
- ^ Ebbers, T., Kool, R. B., Smeele, L. E., Dirven, R., Besten, C. a. D., Karssemakers, L., Verhoeven, T., Herruer, J. M., Van Den Broek, G. B., & Takes, R. P. (2022). The impact of structured and standardized documentation on documentation quality; A multicenter, retrospective study. Journal of Medical Systems, 46(7). https://doi.org/10.1007/s10916-022-01837-9.
- ^ Kruse, C.S., Smith, B., Vanderlinden, H. and Nealand, A. (2018). Security Techniques for the Electronic Health Records. Journal of Medical Systems, 41(8). doi:https://doi.org/10.1007/s10916-017-0778-4.
- ^ Muralidhar, D., Ezhumalai, S., Dhanasekarapandian, R., & Nikketha, B. (2018). Group interventions. Indian Journal of Psychiatry, 60(8), 514. https://doi.org/10.4103/psychiatry.indianjpsychiatry_42_18.
- ^ Kariotis, T.C., Prictor, M., Chang, S. and Gray, K. (2022). Impact of Electronic Health Records on Information Practices in Mental Health Contexts: Scoping Review. Journal of Medical Internet Research, 24(5), p.e30405. doi:https://doi.org/10.2196/30405.
